| In vitro: |
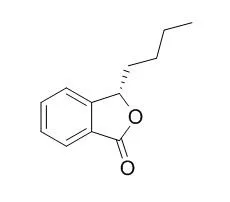
| Drug Metab Dispos. 2014 Apr;42(4):774-81. | | Bioactivation of 3-n-butylphthalide via sulfation of its major metabolite 3-hydroxy-NBP: mediated mainly by sulfotransferase 1A1.[Pubmed: 24468743] | 3-n-Butylphthalide (NBP) [(±)-3-butyl-1(3H)-isobenzofuranone] is an anti-cerebral-ischemia drug. Moderate hepatotoxicity has been observed in clinical applications. One of the major metabolites, 3-N-acetylcysteine-3-n-Butylphthalide, has been detected in human urine, indicating the formation of a reactive metabolite.
METHODS AND RESULTS:
We elucidated the formation mechanism of the reactive metabolite and its association with the hepatotoxicity of 3-n-Butylphthalide. The in vitro incubations revealed that 3-glutathione-3-n-Butylphthalide (3-GSH-NBP) was observed only in fresh rat liver homogenate rather than in liver microsomes, liver cytosol, or liver 9,000g supernatant supplemented with NADPH and GSH. We also detected 3-GSH-3-n-Butylphthalide when 3'-phosphoadenosine-5'-phosphosulfate was added in GSH-fortified human liver cytosol (HLC). The formation of 3-GSH-3-n-Butylphthalide was 39.3-fold higher using 3-hydroxy-3-n-Butylphthalide (3-OH-NBP) as the substrate than 3-n-Butylphthalide. The sulfotransferase (SULT) inhibitors DCNP (2,6-dichloro-4-nitrophenol) and quercetin suppressed 3-GSH-3-n-Butylphthalide formation in HLC by 75 and 82%, respectively, suggesting that 3-OH-NBP sulfation was involved in 3-GSH-3-n-Butylphthalide formation. Further SULT phenotyping revealed that SULT1A1 is the major isoform responsible for the sulfation. Dose-dependent toxicity was observed in primary rat hepatocytes exposed to 3-OH-3-n-Butylphthalide, with an IC50 of approximately 168 μM. Addition of DCNP and quercetin significantly increased cell viability, whereas l-buthionine-sulfoximine (a GSH depleter) decreased cell viability.
CONCLUSIONS:
Overall, our study revealed the underlying mechanism for the bioactivation of NBP is as follows. 3-n-Butylphthalide is first oxidized to 3-OH-3-n-Butylphthalide and further undergoes sulfation to form 3-OH-3-n-Butylphthalide sulfate. The sulfate spontaneously cleaves off, generating highly reactive electrophilic cations, which can bind either to GSH to detoxify or to hepatocellular proteins to cause undesirable side effects. |
|
| In vivo: |
| Alzheimers Dement. 2015 Jun 15. | | The effects of DL-3-n-butylphthalide in patients with vascular cognitive impairment no dementia caused by subcortical ischemic small vessel disease: A multicentre, randomized, double-blind, placebo-controlled trial.[Pubmed: 26086183] | Vascular cognitive impairment without dementia is very common among the aged and tends to progress to dementia, but there have been no proper large-scale intervention trials dedicated to it. Vascular cognitive impairment without dementia caused by subcortical ischemic small vessel disease (hereinafter, subcortical Vascular cognitive impairment without dementia) represents a relatively homogeneous disease process and is a suitable target for therapeutic trials investigating Vascular cognitive impairment without dementia. Preclinical trials showed that dl-3-n-Butylphthalide (NBP) is effective for cognitive impairment of vascular origin.
METHODS AND RESULTS:
In this randomized, double-blind, placebo-controlled trial, we enrolled patients aged 50-70 years who had a diagnosis of subcortical Vascular cognitive impairment without dementia at 15 academic medical centers in China. Inclusion criteria included a clinical dementia rating ≥0.5 on at least one domain and global score ≤0.5; a mini-mental state examination score ≥20 (primary school) or ≥24 (junior school or above); and brain magnetic resonance imaging consistent with subcortical ischemic small vessel disease. Patients were randomly assigned to NBP 200 mg three times daily or matched placebo (1:1) for 24 weeks according to a computer-generated randomization protocol. All patients and study personnel were masked to treatment assignment. Primary outcome measures were the changes in Alzheimer's disease assessment scale-cognitive subscale (ADAS-cog) and clinician's interview-based impression of change plus caregiver input (CIBIC-plus) after 24 weeks. All patients were monitored for adverse events (AEs). Outcome measures were analyzed for both the intention-to-treat (ITT) population and the per protocol population.
This study enrolled 281 patients. NBP showed greater effects than placebo on ADAS-cog (NBP change -2.46 vs. placebo -1.39; P = .03; ITT) and CIBIC-plus (80 [57.1%] vs. 59 [42.1%] patients improved; P = .01; ITT). NBP-related AE were uncommon and primarily consisted of mild gastrointestinal symptoms.
CONCLUSIONS:
Over the 6-month treatment period, NBP was effective for improving cognitive and global functioning in patients with subcortical vascular cognitive impairment without dementia and exhibited good safety. | | Acta Pharmacol Sin. 2015 Jun 15. | | The edaravone and 3-n-butylphthalide ring-opening derivative 10b effectively attenuates cerebral ischemia injury in rats.[Pubmed: 26073328] | Compound 10b is a hybrid molecule of edaravone and a ring-opening derivative of 3-n-Butylphthalide (NBP). The aim of this study was to examine the effects of compound 10b on brain damage in rats after focal cerebral ischemia.
METHODS AND RESULTS:
SD rats were subjected to 2-h-middle cerebral artery occlusion (MCAO). At the onset of reperfusion, the rats were orally treated with 3-n-Butylphthalide (60 mg/kg), edaravone (3 mg/kg), 3-n-Butylphthalide (60 mg/kg)+edaravone (3 mg/kg), or compound 10b (70, 140 mg/kg). The neuroprotective effects of compound 10b were more pronounced compared to 3-n-Butylphthalide, edaravone or 3-n-Butylphthalide+edaravone. Furthermore, compound 10b significantly upregulated the protein levels of the cytoprotective molecules Bcl-2, HO-1, Nrf2, Trx, P-NF-κB p65, and IκB-α, while decreasing the expression of Bax, caspase 3, caspase 9, Txnip, NF-κB p65, and P-IκB-α.
CONCLUSIONS:
Oral administration of compound 10b effectively attenuates rat cerebral ischemia injury. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)