| In vivo: |
| Med Sci Monit. 2014 Mar 11;20:399-405. | | L-carnosine alters some hemorheologic and lipid peroxidation parameters in nephrectomized rats.[Pubmed: 24614724] | Chronic kidney disease (CKD) is a major health problem worldwide. Oxidative stress is one of the mediators of this disease. Systemic complications of oxidative stress are involved in the pathogenesis of hypertension, endothelial dysfunction, shortened erythrocyte lifespan, deformability, and nitric oxide (NO) dysfunction. L-carnosine is known as an antioxidant. In this study, our aim was to investigate the effect of carnosine on hemorheologic and cardiovascular parameters in CKD-induced rats.
METHODS AND RESULTS:
We used 4-month-old male Sprague-Dawley rats divided into 4 groups of 6 rats each. Three days after subtotal nephrectomy and sham operations, the surviving rats were divided into the 4 groups; 1) Sham (S), 2) Sham+Carnosine (S-C), 3) Subtotal nephrectomy (Nx), and 4) Subtotal nephrectomy + Carnosine (N-C). Carnosine was injected intraperitoneally (i.p.) (50 mg/kg) for 15 days. The control group received the same volume of physiological saline.
In CKD rats, malondialdehyde (MDA) levels were increased, and NO and RBC deformability were decreased compared to Sham. Carnosine treatment decreased MDA levels, improved RBC (red blood cell) ability to deform, and increased NO levels. However, carnosine did not affect blood pressure levels in these rats.
CONCLUSIONS:
We found that carnosine has beneficial effects on CKD in terms of lipid peroxidation and RBC deformability. Carnosine may have a healing effect in microcirculation level, but may not have any effect on systemic blood pressure in CKD-induced rats.
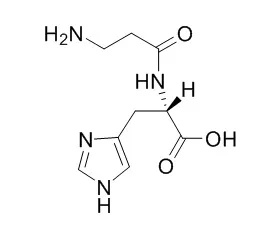
| | Exp Eye Res. 2013 Aug;113:135-42. | | Β-alanine and l-histidine transport across the inner blood-retinal barrier: potential involvement in L-carnosine supply.[Pubmed: 23773890] | The supply of L-carnosine, a bioactive dipeptide of β-alanine and l-histidine, to the retina across the blood-retinal barrier (BRB) was studied.
METHODS AND RESULTS:
The in vivo and in vitro studies revealed low uptake activities for [(3)H]Gly-Sar, a representative dipeptide, suggesting that L-carnosine transport plays only a minor role at the BRB. The in vivo study using rats showed approximately 18- and 23-fold greater retinal uptake indexes (RUI) for [(3)H]β-alanine and [(3)H]l-histidine compared with that of a paracellular marker, respectively. The RUI of [(3)H]β-alanine was taurine- and γ-aminobutyric acid-sensitive, and the in vitro uptake by TR-iBRB2 cells showed time- concentration- and temperature-dependent [(3)H]β-alanine uptake, suggesting that a carrier-mediated process was involved in β-alanine transport across the inner BRB. [(3)H]β-Alanine uptake was inhibited by taurine and β-guanidinopropionic acid, suggesting that taurine transporter (TAUT/SLC6A6) is responsible for the influx transport of β-alanine across the inner BRB. Regarding l-histidine, the l-leucine-sensitive RUI of [(3)H]l-histidine was identified, and the in vitro [(3)H]l-histidine uptake by TR-iBRB2 cells suggested that a carrier-mediated process was involved in l-histidine transport across the inner BRB. The inhibition profile suggested that L-type amino acid transporter (LAT1/SLC7A5) is responsible for the influx transport of l-histidine across the inner BRB.
CONCLUSIONS:
These results show that the influx transports of β-alanine and l-histidine across the inner BRB is carried out by TAUT and LAT1, respectively, suggesting that the retinal L-carnosine is supplied by enzymatic synthesis from two kinds of amino acids transported across the inner BRB. | | Nutr Clin Pract. 2013 Oct;28(5):609-16. | | Effects of L-carnosine and its zinc complex (Polaprezinc) on pressure ulcer healing.[Pubmed: 23835365] | L-carnosine (CAR) is an endogenous dipeptide. We aimed to determine the effects of CAR and its zinc complex polaprezinc (PLZ) on pressure ulcer healing in institutionalized long-term care patients.
METHODS AND RESULTS:
This study was a nonrandomized controlled trial with a maximum 4-week follow-up. Forty-two patients with stage II-IV pressure ulcers for 4 or more weeks were allocated to 1 of 3 groups in order of recruitment: the control group (n = 14) was untreated, the PLZ group (n = 10) orally received 150 mg/d PLZ (containing 116 mg CAR and 34 mg zinc), and the CAR group (n = 18) orally received 116 mg/d CAR. Pressure ulcer severity was measured weekly using the Pressure Ulcer Scale for Healing (PUSH) score.
At baseline, no significant differences were found among groups in demographic and nutrition parameters and pressure ulcer characteristics (severity, size, and staging). After 4 weeks, the rate of pressure ulcer healing, assessed by the mean weekly improvement in PUSH score, was significantly greater in the CAR (1.6 ± 0.2, P = .02) and PLZ groups (1.8 ± 0.2, P = .009) than in the control group (0.8 ± 0.2). The difference between the CAR and PLZ groups was not significant (P = .73). Actual dietary intakes over this period did not differ significantly among groups.
CONCLUSIONS:
Our results suggest that CAR and PLZ may almost equally accelerate pressure ulcer healing during 4 weeks. The results need confirmation by randomized controlled trials with larger sample sizes. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)