| In vitro: |
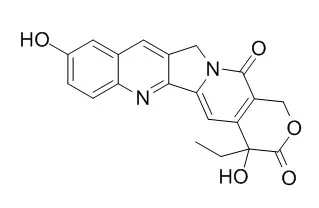
| J Drug Target. 2015 Mar 13:1-6. | | Intracellular target delivery of 10-hydroxycamptothecin with solid lipid nanoparticles against multidrug resistance.[Pubmed: 25766079] | The main objective of this study was to design a suitable drug delivery system for 10-Hydroxycamptothecin (HCPT).
METHODS AND RESULTS:
In this study, HCPT-loaded solid lipid nanoparticle (HCPT-loaded SLN) was successfully prepared. The HCPT-loaded SLN was characterized by size, entrapment efficiency and drug release manner. The cytotoxicity of HCPT-loaded SLN was assessed in vitro using HepG2/HCPT cells and in vivo utilizing human tumor xenograft nude mouse model. HCPT-loaded SLN indicated the ability to target HepG2/HCPT cells and accumulated higher drug content in HepG2/HCPT cells. HCPT-loaded SLN enhanced the cytotoxicity of HCPT in a concentration-dependent manner.
CONCLUSIONS:
Based on these results, HCPT-loaded SLN suggested being a promising vehicle for liver-targeted drug delivery. Moreover, it can be of clinical interest to overcome multidrug resistance (MDR) effectively. | | Life Sci. 2001 Aug 24;69(14):1619-28. | | Antiangiogenic potential of 10-hydroxycamptothecin.[Pubmed: 11589502] |
METHODS AND RESULTS:
To investigate the antiangiogenic potential of 10-Hydroxycamptothecin (HCPT), the proliferation of human microvascular endothelial cells (HMEC) and seven human tumor cell lines were detected by SRB assay, and the endothelial cell migration and tube formation were assessed using two in vitro model systems. Also, inhibition of angiogenesis was determined with a modification of the chick embryo chorioallantoic membrane (CAM) assay in vivo. Morphological assessment of apoptosis was performed by fluorescence microscope. HCPT 0.313-5 micromol x L(-1) treatment resulted in a dose-dependent inhibition of proliferation, migration and tube formation in HMEC cells, and HCPT 6.25-25 nmol x egg(-1) inhibited angiogenesis in CAM assay. HCPT 1.25-5 micromol x L(-1) elicited typical morphological changes of apoptosis including condensed chromatin, nuclear fragmentation, and reduction in volume in HMEC cells. HCPT significantly inhibited angiogenesis both in vitro and in vivo at relatively low concentrations, and this effect was related with induction of apoptosis in HMEC cells.
CONCLUSIONS:
These results taken collectively suggest that HCPT may be a potent antiangiogenetic and cytotoxic drug and further investigation is warranted. |
|
| In vivo: |
| Cancer Chemother Pharmacol. 1998;41(4):257-67. | | Preclinical pharmacology of the natural product anticancer agent 10-hydroxycamptothecin, an inhibitor of topoisomerase I.[Pubmed: 9488594 ] | 10-Hydroxycamptothecin (HCPT) is an indole alkaloid isolated from a Chinese tree, Camptotheca acuminata, and has a wide spectrum of anticancer activity in vitro and in vivo mainly through inhibitory effects on topoisomerase I. HCPT has been shown to be more potent and less toxic than camptothecin and has recently undergone clinical trials. To determine how HCPT might be best used as an anticancer agent, preclinical studies of the pharmacokinetics, tissue distribution, metabolism and elimination of HCPT in rats were undertaken.
METHODS AND RESULTS:
HCPT was administered to rats by i.v. bolus injection at doses of 1, 3, and 10 mg/kg body weight. HCPT (lactone and carboxylate) and its metabolites in plasma, urine, feces, and various tissues were quantitated by reversed-phase HPLC. Pharmacokinetic parameters were then estimated.
Following i.v. administration at doses of 3 or 10 mg/kg, the plasma concentration-time profile for lactone HCPT could be best described by a three-compartment model, with terminal elimination half-lives of 140.4 and 428.6 min, respectively. A two-compartment model was used to fit the plasma concentration-time curve at 1 mg/kg, with a terminal elimination half-life of 30.5 min. Carboxylate HCPT had a longer half-life than the lactone form of HCPT. During the initial 6 h after dosing, urinary excretion was the major route of elimination, and fecal excretion became the major route of elimination thereafter. HCPT was widely distributed to various tissues including the enterohepatic system, kidney, and bone marrow. The lactone form of HCPT was detectable in various tissues examined up to 72 h after dosing at all the three test doses. HCPT glucuronides were present in plasma, urine, feces and various tissues. No significant toxicity was observed at doses of 1 or 3 mg/kg. Polyuria and hematuria were observed only during the initial 3 h after dosing at 10 mg/kg.
CONCLUSIONS:
Prolonged elimination of HCPT in vivo may have a significant impact on its therapeutic effects. HCPT is metabolized to its carboxylate form and glucuronides. Dose-dependent toxicity was observed with i.v. administration of HCPT. The results of this study should be useful in the design of future human trials with this anticancer drug. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)