| Kinase Assay: |
| Aging Cell. 2015 Aug;14(4):569-81. | | Relation between TLR4/NF-κB signaling pathway activation by 27-hydroxycholesterol and 4-hydroxynonenal, and atherosclerotic plaque instability.[Pubmed: 25757594] | It is now thought that atherosclerosis, although due to increased plasma lipids, is mainly the consequence of a complicated inflammatory process, with immune responses at the different stages of plaque development. Increasing evidence points to a significant role of Toll-like receptor 4 (TLR4), a key player in innate immunity, in the pathogenesis of atherosclerosis.
METHODS AND RESULTS:
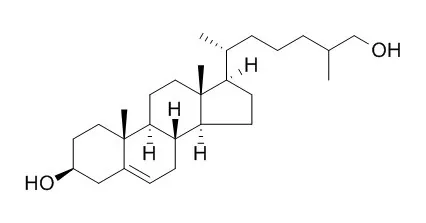
This study aimed to determine the effects on TLR4 activation of two reactive oxidized lipids carried by oxidized low-density lipoproteins, the oxysterol 27-Hydroxycholesterol (27-OH) and the aldehyde 4-hydroxynonenal (HNE), both of which accumulate in atherosclerotic plaques and play a key role in the pathogenesis of atherosclerosis. Secondarily, it examined their potential involvement in mediating inflammation and extracellular matrix degradation, the hallmarks of high-risk atherosclerotic unstable plaques. In human promonocytic U937 cells, both 27-OH and HNE were found to enhance cell release of IL-8, IL-1β, and TNF-α and to upregulate matrix metalloproteinase-9 (MMP-9) via TLR4/NF-κB-dependent pathway; these actions may sustain the inflammatory response and matrix degradation that lead to atherosclerotic plaque instability and to their rupture. Using specific antibodies, it was also demonstrated that these inflammatory cytokines increase MMP-9 upregulation, thus enhancing the release of this matrix-degrading enzyme by macrophage cells and contributing to plaque instability.
CONCLUSIONS:
These innovative results suggest that, by accumulating in atherosclerotic plaques, the two oxidized lipids may contribute to plaque instability and rupture. They appear to do so by sustaining the release of inflammatory molecules and MMP-9 by inflammatory and immune cells, for example, macrophages, through activation of TLR4 and its NF-κB downstream signaling. |
|
| Animal Research: |
| J Hepatol. 2015 Feb;62(2):430-6. | | Hematopoietic overexpression of Cyp27a1 reduces hepatic inflammation independently of 27-hydroxycholesterol levels in Ldlr(-/-) mice.[Pubmed: 25281859 ] | Non-alcoholic steatohepatitis (NASH) is characterized by hepatic lipid accumulation and inflammation. Currently, the underlying mechanisms, leading to hepatic inflammation, are still unknown. The breakdown of free cholesterol inside Kupffer cells (KCs) by the mitochondrial enzyme CYP27A1 produces 27-Hydroxycholesterol (27HC). We recently demonstrated that administration of 27HC to hyperlipidemic mice reduced hepatic inflammation. In line, hematopoietic deletion of Cyp27a1 resulted in increased hepatic inflammation. In the current manuscript, the effect of hematopoietic overexpression of Cyp27a1 on the development of NASH and cholesterol trafficking was investigated. We hypothesized that Cyp27a1 overexpression in KCs will lead to reduced hepatic inflammation.
METHODS AND RESULTS:
Irradiated Ldlr(-/-) mice were transplanted (tp) with bone marrow from mice overexpressing Cyp27a1 (Cyp27a1(over)) and wild type (Wt) mice and fed either chow or a high-fat, high-cholesterol (HFC) diet for 3 months. Additionally, gene expression was assessed in bone marrow-derived macrophages (BMDM) from Cyp27a1(over) and Wt mice.
In line with our hypothesis, hepatic inflammation in HFC-fed Cyp27a1(over)-tp mice was reduced and KCs were less foamy compared to Wt-tp mice. Remarkably, these changes occurred even though plasma and liver levels of 27HC did not differ between both groups. BMDM from Cyp27a1(over) mice revealed reduced inflammatory gene expression and increased expression of cholesterol transporters compared to Wt BMDM after lipopolysaccharide (LPS) stimulation.
CONCLUSIONS:
Our data suggest that overexpression of Cyp27a1 in KCs reduces hepatic inflammation independently of 27HC levels in plasma and liver, further pointing towards KCs as specific target for improving the therapy of NASH. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)