| In vitro: |
| Cell Biochem Biophys. 2013 Sep;67(1):199-206. | | Gambogic acid sensitizes ovarian cancer cells to doxorubicin through ROS-mediated apoptosis.[Pubmed: 23436279] | Ovarian cancer is one human malignancy which has response portly to doxorubicin. The anti-cancer activity of Gambogic acid has been tested in in vitro and in vivo studies.
METHODS AND RESULTS:
In this study, we showed that Gambogic acid, a natural compound, could potentiate the anticancer activity of doxorubicin in ovarian cancer through ROS-mediated apoptosis. Platinum-resistant human ovarian cancer cell line (SKOV-3) was treated with Gambogic acid, doxorubicin, or the combination of both to investigate cell proliferation and apoptosis. We found that the combination of Gambogic acid and doxorubicin causes synergistic loss of cell viability in SKOV-3 cells and this synergistic effect correlated with increased cellular ROS accumulation. Moreover, in vivo results showed that Gambogic acid and doxorubicin combination resulted in a synergistic suppressing effect on tumor growth in ovarian cancer mice model.
CONCLUSIONS:
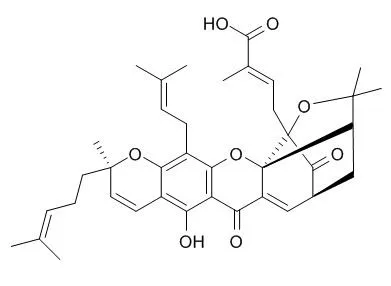
Taken together, the results suggested that doxorubicin in combination with Gambogic acid might provide a promising therapeutic strategy to enhance chemosensitivity of ovarian cancer to doxorubicin. | | Cancer Res. 2008 Mar 15;68(6):1843-50. | | Gambogic acid inhibits angiogenesis and prostate tumor growth by suppressing vascular endothelial growth factor receptor 2 signaling.[Pubmed: 18339865 ] | Gambogic acid (GA), the main active compound of Gamboge hanburyi, has been previously reported to activate apoptosis in many types of cancer cell lines by targeting transferrin receptor and modulating nuclear factor-kappaB signaling pathway. Whether GA inhibits angiogenesis, which is crucial for cancer and other human diseases, remains unknown.
METHODS AND RESULTS:
Here, we found that GA significantly inhibited human umbilical vascular endothelial cell (HUVEC) proliferation, migration, invasion, tube formation, and microvessel growth at nanomolar concentration. In a xenograft prostate tumor model, we found that GA effectively inhibited tumor angiogenesis and suppressed tumor growth with low side effects using metronomic chemotherapy with GA. GA was more effective in activating apoptosis and inhibiting proliferation and migration in HUVECs than in human prostate cancer cells (PC3), suggesting GA might be a potential drug candidate in cancer therapy through angioprevention with low chemotoxicity. Furthermore, we showed that GA inhibited the activations of vascular endothelial growth factor receptor 2 and its downstream protein kinases, such as c-Src, focal adhesion kinase, and AKT.
CONCLUSIONS:
Together, these data suggest that GA inhibits angiogenesis and may be a viable drug candidate in antiangiogenesis and anticancer therapies. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)