Natural Products

- ChemFaces is a professional high-purity natural products manufacturer.
- Product Intended Use
- 1. Reference standards
- 2. Pharmacological research
- 3. Inhibitors



| Size /Price /Stock | 10 mM * 1 mL in DMSO / $10.8 / In-stock | Other Packaging | *Packaging according to customer requirements(100uL/well, 200uL/well and more), and Container use Storage Tube With Screw Cap |

| Size /Price /Stock | 10 mM * 100 uL in DMSO / Inquiry / In-stock 10 mM * 1 mL in DMSO / Inquiry / In-stock | Related Libraries |
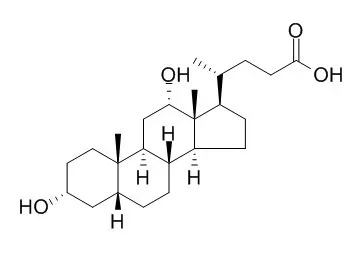
| Description: | Deoxycholic acid is a strong promoter of hepatocarcinogenesis with possible complete carcinogenicity in the liver and promotion potential for tumor development in the small intestine. Loss of deoxycholic acid-induced EGFR/Ras/MAPK pathway function potentiates deoxycholic acid-stimulated FAS-induced hepatocyte cell death via a reduction in the expression of c-FLIP isoforms. |
| Targets: | EGFR | MAPK | MEK | Caspase | PI3K | Ras | c-FLIP |
| Source: | The bile of Pig |
| Solvent: | Chloroform, Dichloromethane, Ethyl Acetate, DMSO, Acetone, etc. |
| Storage: | Providing storage is as stated on the product vial and the vial is kept tightly sealed, the product can be stored for up to 24 months(2-8C). Wherever possible, you should prepare and use solutions on the same day. However, if you need to make up stock solutions in advance, we recommend that you store the solution as aliquots in tightly sealed vials at -20C. Generally, these will be useable for up to two weeks. Before use, and prior to opening the vial we recommend that you allow your product to equilibrate to room temperature for at least 1 hour. Need more advice on solubility, usage and handling? Please email to: service@chemfaces.com |
| After receiving: | The packaging of the product may have turned upside down during transportation, resulting in the natural compounds adhering to the neck or cap of the vial. take the vial out of its packaging and gently shake to let the compounds fall to the bottom of the vial. for liquid products, centrifuge at 200-500 RPM to gather the liquid at the bottom of the vial. try to avoid loss or contamination during handling. |
 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.5473 mL | 12.7366 mL | 25.4732 mL | 50.9463 mL | 63.6829 mL |
| 5 mM | 0.5095 mL | 2.5473 mL | 5.0946 mL | 10.1893 mL | 12.7366 mL |
| 10 mM | 0.2547 mL | 1.2737 mL | 2.5473 mL | 5.0946 mL | 6.3683 mL |
| 50 mM | 0.0509 mL | 0.2547 mL | 0.5095 mL | 1.0189 mL | 1.2737 mL |
| 100 mM | 0.0255 mL | 0.1274 mL | 0.2547 mL | 0.5095 mL | 0.6368 mL |
| Citation [1] Carcinogenesis. 1988 Jun;9(6):1103-5. | Positive influence of dietary deoxycholic acid on development of pre-neoplastic lesions initiated by N-methyl-N-nitrosourea in rat liver.[Pubmed: 3370752] |
| The effect of Deoxycholic acid (DCA) treatment subsequent to initiation of F344 male rats with N-methyl-N-nitrosourea (MNU), a wide spectrum carcinogen inducing tumors in many organs, was investigated. Rats were initially given four doses of MNU (50 mg/kg) i.p. within a 2-week period combined with a two-thirds partial hepatectomy performed at day 7 and then placed on basal diet containing DCA at concentrations of 0.313, 0.125, 0.050 and 0.020% for 21 weeks prior to final sacrifice. All organs studied were carefully examined histologically and histochemically for development of neoplastic and pre-neoplastic lesions. DCA enhanced the induction of glutathione S-transferase positive (GST-P+) liver cell foci in a dose-related manner. Furthermore groups of rats given DCA without prior MNU administration also developed dose-dependent numbers of pre-neoplastic liver lesions. In addition, increased numbers of small intestine tumors were apparent in DCA-treated animals although the difference was not significant. Induction of tumors in the thyroids, Zymbal glands, skin and peripheral nerves was not affected. The results indicate that DCA is a strong promoter of hepatocarcinogenesis with possible complete carcinogenicity in the liver and promotion potential for tumor development in the small intestine. | |
| Citation [2] Mol. Biol. Cell., 2001,12(9):2629-45. | Deoxycholic Acid (DCA) Causes Ligand-independent Activation of Epidermal Growth Factor Receptor (EGFR) and FAS Receptor in Primary Hepatocytes: Inhibition of EGFR/Mitogen-activated Protein Kinase-Signaling Module Enhances DCA-induced Apoptosis[Reference: WebLink] |
| Previous studies have argued that enhanced activity of the epidermal growth factor receptor (EGFR) and the mitogen-activated protein kinase (MAPK) pathway can promote tumor cell survival in response to cytotoxic insults. In this study, we examined the impact of MAPK signaling on the survival of primary hepatocytes exposed to low concentrations of Deoxycholic acid (DCA, 50 μM). Treatment of hepatocytes with DCA caused MAPK activation, which was dependent upon ligand independent activation of EGFR, and downstream signaling through Ras and PI3 kinase. Neither inhibition of MAPK signaling alone by MEK1/2 inhibitors, nor exposure to DCA alone, enhanced basal hepatocyte apoptosis, whereas inhibition of DCA-induced MAPK activation caused ~25% apoptosis within 6 h. Similar data were also obtained when either dominant negative EGFR-CD533 or dominant negative Ras N17 were used to block MAPK activation. DCA-induced apoptosis correlated with sequential cleavage of procaspase 8, BID, procaspase 9, and procaspase 3. Inhibition of MAPK potentiated bile acid-induced apoptosis in hepatocytes with mutant FAS-ligand, but did not enhance in hepatocytes that were null for FAS receptor expression. These data argues that DCA is causing ligand independent activation of the FAS receptor to stimulate an apoptotic response, which is counteracted by enhanced ligand-independent EGFR/MAPK signaling. In agreement with FAS-mediated cell killing, inhibition of caspase function with the use of dominant negative Fas-associated protein with death domain, a caspase 8 inhibitor (Ile-Glu-Thr-Asp-p-nitroanilide [IETD]) or dominant negative procaspase 8 blocked the potentiation of bile acid-induced apoptosis. Inhibition of bile acid-induced MAPK signaling enhanced the cleavage of BID and release of cytochrome cfrom mitochondria, which were all blocked by IETD. Despite activation of caspase 8, expression of dominant negative procaspase 9 blocked procaspase 3 cleavage and the potentiation of DCA-induced apoptosis. Treatment of hepatocytes with DCA transiently increased expression of the caspase 8 inhibitor proteins c-FLIP-S and c-FLIP-L that were reduced by inhibition of MAPK or PI3 kinase. Constitutive overexpression of c-FLIP-s abolished the potentiation of bile acid-induced apoptosis. Collectively, our data argue that loss of DCA-induced EGFR/Ras/MAPK pathway function potentiates DCA-stimulated FAS-induced hepatocyte cell death via a reduction in the expression of c-FLIP isoforms. | |
| Citation [3] J Cosmet Dermatol. 2015 Mar;14(1):33-9. | A phase 1 pharmacokinetic study of ATX-101: serum lipids and adipokines following synthetic deoxycholic acid injections.[Pubmed: 25684122] |
| BACKGROUND: ATX-101 (Deoxycholic acid injection, Kythera Biopharmaceuticals, Inc.) is a proprietary formulation of pure synthetic Deoxycholic acid (DCA). It is undergoing clinical investigation as an injectable drug for contouring the submental area by reducing submental fat (SMF). When injected into subcutaneous fat, ATX-101 causes focal adipocytolysis, the targeted destruction of fat cells. OBJECTIVES: This phase 1 study evaluated the safety, pharmacokinetics (PK), and pharmacodynamic effects of ATX-101 (100-mg total dose). METHODS: Following PK evaluation of baseline endogenous Deoxycholic acid , lipids, and adipokines in the initial stage of the study (samples collected at hours 0.25, 0.5, 1, 1.5, 2, 4, 6, 12, 15.5, and 24.5), 10 subjects received subcutaneous injections of ATX-101 into abdominal fat. PK evaluation of DCA, lipids, and adipokines was repeated in the second phase of the study. RESULTS: After ATX-101 injections, plasma concentration of Deoxycholic acid increased transiently, reached a maximum plasma concentration rapidly, and returned to endogenous concentrations within 12 h postdose. ATX-101 injection was not associated with any clinically meaningful changes in systemic concentrations of total cholesterol, total triglycerides, free fatty acids, C-reactive protein, or interleukin-6. Adverse events were mild in severity, transient, and showed a temporal relationship to dosing. CONCLUSIONS: This study demonstrated favorable safety and PK profiles, and no clinically meaningful changes in Deoxycholic acid , lipids, and proinflammatory cytokines following subcutaneous injection of ATX-101. Our results support continued clinical investigation of ATX-101 as an injectable drug to reduce SMF. | |
| Citation [4] Int J Mol Sci. 2015 Mar 31;16(4):7195-209. | In vitro investigation of self-assembled nanoparticles based on hyaluronic acid-deoxycholic acid conjugates for controlled release doxorubicin: effect of degree of substitution of deoxycholic acid.[Pubmed: 25837468 ] |
| Self-assembled nanoparticles based on a hyaluronic acid-Deoxycholic acid (HD) chemical conjugate with different degree of substitution (DS) of Deoxycholic acid (DOCA) were prepared. The degree of substitution (DS) was determined by titration method. The nanoparticles were loaded with doxorubicin (DOX) as the model drug. The human cervical cancer (HeLa) cell line was utilized for in vitro studies and cell cytotoxicity of DOX incorporated in the HD nanoparticles was accessed by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. In addition, cellular uptake of fluorescently labeled nanoparticles was also investigated. An increase in the degree of Deoxycholic acid substitution reduced the size of the nanoparticles and also enhanced their drug encapsulation efficiency (EE), which increased with the increase of DS. A higher degree of Deoxycholic acid substitution also lead to a lower release rate and an initial burst release of doxorubicin from the nanoparticles. In summary, the degree of substitution allows the modulation of the particle size, drug encapsulation efficiency, drug release rate, and cell uptake efficiency of the nanoparticles. The herein developed hyaluronic acid-Deoxycholic acid conjugates are a good candidate for drug delivery and could potentiate therapeutic formulations for doxorubicin-mediated cancer therapy. |