| In vivo: |
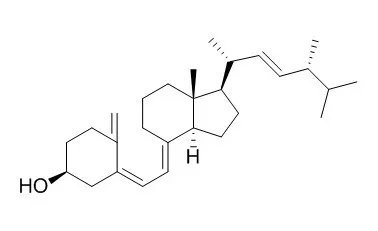
| Clin J Am Soc Nephrol. 2012 Feb;7(2):216-23. | | Ergocalciferol supplementation in children with CKD delays the onset of secondary hyperparathyroidism: a randomized trial.[Pubmed: 22266572 ] | Vitamin D deficiency is an important contributor to the development of hyperparathyroidism and is independently associated with cardiovascular and bone disease. The hypothesis was that nutritional vitamin D (Ergocalciferol) supplementation in children with CKD stages 2-4 delays the onset of secondary hyperparathyroidism.
METHODS AND RESULTS:
A randomized, double-blinded, placebo-controlled study in children with CKD2-4 who had 25-hydroxyvitamin D [25(OH)D] deficiency was conducted. Ergocalciferol (or a matched placebo) was given daily as per Kidney Disease Outcomes Quality Initiative guidelines. The primary endpoint was the time to development of hyperparathyroidism.
Seventy-two children were screened. Forty-seven children were 25(OH)D-deficient and randomly assigned to receive Ergocalciferol or placebo. Twenty children in each arm completed the study; median follow-up was 12 months. Groups were well matched for age, race, estimated GFR, and season when recruited. Nine of 20 children on placebo and 3 of 20 children on Ergocalciferol developed hyperparathyroidism (odds ratio, 4.64; 95% confidence interval, 1.02-21.00). The time to development of hyperparathyroidism was significantly longer with Ergocalciferol treatment compared with placebo (hazard ratio, 0.30; 95% confidence interval, 0.09-0.93, P=0.05). With Ergocalciferol treatment, normal 25(OH)D levels were achieved in all 8 children with CKD2, 8 of 11 children with CKD3, but not in the single patient with CKD4. There were no Ergocalciferol-related adverse events. 25(OH)D levels >100 nmol/L were required to achieve normal levels of 1,25-dihydroxyvitamin D.
CONCLUSIONS:
Ergocalciferol is an effective treatment that delays the development of secondary hyperparathyroidism in children with CKD2-3. | | Pediatr Nephrol. 2013 Aug;28(8):1261-6. | | Ergocalciferol decreases erythropoietin resistance in children with chronic kidney disease stage 5.[Pubmed: 23420502] | Vitamin D(Ergocalciferol) insufficiency is related to erythropoietin resistance in chronic kidney disease (CKD). This study was conducted to evaluate the effect of Ergocalciferol on the dose of erythrocyte-stimulating agent (ESA) administered to children with CKD stage 5 and vitamin D insufficiency.
METHODS AND RESULTS:
Twenty patients aged <18 years with CKD stages 5 or 5D and vitamin D insufficiency were divided into two groups. During the 12-week study, ten patients received oral Ergocalciferol (treatment) whereas the other ten patients did not (control). The ESA dosage was recorded monthly.
There were no significant differences in demographic data, ESA dosages, and laboratory data, including corrected calcium, phosphorus, parathyroid hormone, hemoglobin, ferritin, 25-hydroxyvitamin D (25D), and transferrin saturation levels, between the two groups at baseline. At the completion of the study, serum 25D levels in the treatment group were significantly increased from baseline (p = 0.02) and were significantly higher than the serum 25D levels in the controls (p < 0.005). The ESA dosage in the treatment group was significantly decreased when compared to baseline (p = 0.04).
CONCLUSIONS:
Vitamin D deficiency should be routinely detected and treated. Our results show that the administration of Ergocalciferol in conjunction with 1,25-dihydroxyvitamin D3 reduced the dose of ESA required to treat children with CKD stages 5 and 5D and may decrease erythropoietin resistance. | | Scand J Clin Lab Invest. 2013 Mar;73(2):107-16. | | Ergocalciferol treatment and aspects of mineral homeostasis in patients with chronic kidney disease stage 4-5.[Pubmed: 23281842] | Focus on non-classical effects and possible less side effects of treatment with nutritional vitamin D, raises the expectation of possible benefits from treating chronic kidney disease (CKD) patients with Ergocalciferol (vitamin D2). Treatment with 1,25(OH)2 vitamin D (calcitriol) induces elevated fibroblast growth factor 23 (FGF23), while epidemiological studies have found positive effects of nutritional and 25(OH)vitamin D on mortality in CKD. Disturbed mineral homeostasis in CKD is correlated to adverse outcome and cardiovascular mortality. The objective was to examine the possible effects of treatment with high doses of Ergocalciferol on parameters of mineral homeostasis in predialysis CKD patients.
METHODS AND RESULTS:
A total of 43 adult patients with CKD stage 4-5, not receiving vitamin D supplementation, were studied, and allocated by simple randomization to either an intervention (n = 26) or a control group (n = 17). The intervention group received Ergocalciferol, 50.000 IU/week for 6 weeks. Plasma FGF23, creatinine, parathyroid hormone (PTH), phosphate and ionized calcium were obtained at baseline and after the 6 weeks.
The intervention group had a significant increase in 25(OH)D2 concentration from < 10 to 90 ± 4 nmol/L, while 1,25(OH)2D (62 ± 6 at baseline and 67 ± 6 pmol/L at 6 weeks) remained stable. No changes were seen in the circulating vitamin D concentrations in the control group. After the 6 weeks of treatment no significant changes were seen in concentration of creatinine, phosphate, ionized calcium, PTH and FGF23 remained stable.
CONCLUSIONS:
No harmful effects of short-term treatment with high-dose Ergocalciferol were observed on markers of mineral homeostasis and FGF23 in CKD patients stage 4-5. | | Am J Med. 1995 May;98(5):459-63. | | Cyclical etidronate plus ergocalciferol prevents glucocorticoid-induced bone loss in postmenopausal women.[Pubmed: 7733124] | The two groups did not differ with respect to age, years since the menopause, mean daily To assess the benefit of cyclical etidronate plus Ergocalciferol for the prevention of glucocorticoid-induced bone loss in a 2-year, prospective, open study based in an osteoporosis clinic.
METHODS AND RESULTS:
Group 1 consisted of 15 postmenopausal women (mean age 62.6 +/- 3.3 years) who commenced glucocorticoid therapy and were treated with cyclical etidronate (400 mg/d for the first month; thereafter, 400 mg/d for 2 weeks of every 3-month period), elemental calcium (1 g/d), and Ergocalciferol (0.5 mg/wk). Group 2 consisted of 11 postmenopausal women (mean age 60.2 +/- 4.7 years) with glucocorticoid-induced osteoporosis, who were attending the clinic at the same time and were treated with calcium supplements only (1 g/d).
Lumbar spine and femoral neck bone mineral densities (BMD) were measured at baseline and after 12 and 24 months of glucocorticoid therapy using a dual energy x-ray absorptiometer.
The two groups did not differ with respect to age, years since the menopause, mean daily glucocorticoid dose, and baseline BMD values. During the first year of therapy, mean lumbar spine BMD increased from an initial value of 0.88 g/cm2 to 0.94 g/cm2, an increase of 7% per year (95% confidence interval [CI] 3.7% to 10.2%; P < 0.001 compared with controls). Significant increases in BMD of 2.5% per year were also observed in the femoral neck (95% CI -1% to 6%; P < 0.01 compared with controls). After the second year of cyclical etidronate therapy, femoral neck BMD continued to increase (P < 0.05 compared with value at 12 months), while lumbar spine BMD remained stable.
CONCLUSIONS:
Chronic glucocorticoid therapy may result in bone loss at most skeletal sites. Therapy with cyclical etidronate plus Ergocalciferol not only prevented glucocorticoid-induced bone loss, but even increased lumbar spine and femoral neck BMD in postmenopausal women commencing glucocorticoid therapy. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)