| In vivo: |
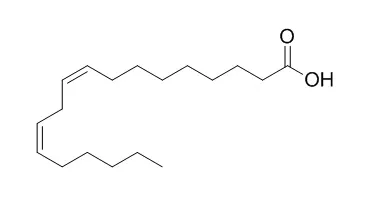
| Clinical Nutrition, 2003, 22(6):529-535. | | Linoleic acid, but not oleic acid, upregulates the production of interleukin-8 by human intestinal smooth muscle cells isolated from patients with Crohn's disease.[Reference: WebLink] | Crohn's disease is a chronic inflammatory bowel disease (IBD) of unknown etiology. In this study, we investigated the hypothesis that dietary fatty acids, Linoleic acid (LA) and oleic acid (OA), could be involved in the inflammatory response through stimulation of the neutrophil chemokine, IL-8.
METHODS AND RESULTS:
Human intestinal smooth muscle (HISM) cells were isolated from normal patients and patients with Crohn's disease and cultured for 24 h with LA or OA in the presence or absence of oxidative stress. The concentrations of IL-8 were measured in the media and cellular oxidative stress was quantitated by measurement of thiobarbituric acid reactive substances (TBARSs). Spontaneous production of IL-8 was significantly higher in HISM cells isolated from Crohn's bowel compared to control bowel. LA caused a marked, nine-fold, increase in IL-8 secretion by Crohn's cells, an effect that could be simulated in normal HISM cells by co-incubation of LA with an oxidizing solution (Ox) composed of hypoxanthine+xanthine oxidase+FeSO4 (OxLA). These effects were inhibited by vitamins C and E. Treatment of Crohn's cells with OxLA did not further increase IL-8 over that of LA alone. The effect of LA alone was not associated with an increase in cellular oxidative stress as quantitated by TBARSs. In contrast to the results with LA, treatment with OA or OxOA did not increase IL-8 in either normal or Crohn's cells. In addition, OA protected Crohn's cells from the increase in TBARSs induced by Ox. In contrast to IL-8, spontaneous production of monocyte chemotactic protein (MCP-1) was significantly lower in Crohn's HISM cells as compared to normal cells and exposure to OxLA did not increase its production.
CONCLUSIONS:
LA, but not OA, increased the production of IL-8 by HISM cells. These results suggest that replacement of LA by OA in the diet of Crohn's patients and increased intake of a diet rich in antioxidants could be beneficial in decreasing inflammatory activity in Crohn's disease. | | Int J Clin Exp Pathol . 2015 May 1;8(5) | | Linoleic acid induces red blood cells and hemoglobin damage via oxidative mechanism[Pubmed: 26191198] | | Abstract
Hidden blood loss typically occurs following total hip arthroplasty (THA) and total knee arthroplasty (TKA) and is thought to be related to free fatty acid (FFA). To study the effect of Linoleic acid on red blood cells and to examine the pathogenesis of hidden blood loss in vivo, we generated an animal model by injecting Linoleic acid into the tail veins of rats. We collected blood samples and determined red blood cell count (RBC) and levels of hemoglobin (Hb), as well as the oxidation and reducing agents in the blood, including glutathione peroxidase (GSH-PX), total superoxide dismutase (T-SOD), hydrogen peroxide (H2O2), and ferryl hemoglobin (Fe4+=O2-), which is generated by the oxidation of Hb. Hidden blood loss occurred when Linoleic acid was administered at a concentration of 60 mmol/L; RBC and Hb levels were significantly reduced by 24 h post-injection. This was followed by erythrocyte deformation, reduced activity of GSH-PX and T-SOD, and decreased levels of H2O2. This was accompanied by an increase in ferryl species, which likely contributes to oxidative stress in vivo. Our findings suggest that Linoleic acid enhances acute red blood cell injury. Hb and RBC began to increase by 72 h, potentially resulting from Linoleic acid metabolism. Thus, elevated levels of Linoleic acid in the blood cause acute oxidative damage to red blood cells, eventually leading to partial acute anemia. These findings highlight the pathophysiology underlying hidden blood loss.
Keywords: Linoleic acid; erythrocyte damage; free fatty acid; hidden blood loss; oxidative stress. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)