| In vivo: |
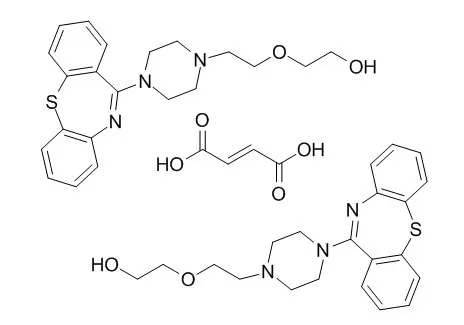
| CNS Neurosci Ther. 2013 Oct;19(10):737-44. | | Quetiapine fumarate for the treatment of multiple sclerosis: focus on myelin repair.[Pubmed: 23870612 ] |
METHODS AND RESULTS:
Quetiapine fumarate is an atypical antipsychotic with reported remyelinating and neuroprotective properties in inflammatory and noninflammatory models of demyelination, including experimental autoimmune encephalomyelitis, and both cuprizone- and global cerebral ischemia-induced demyelination. Preclinical studies suggest that quetiapine may exert these effects by stimulating proliferation and maturation of oligodendrocytes, releasing neurotrophic factors, increasing antioxidant defences, scavenging for free radicals, and inhibiting activated microglia, astrocytes, and T lymphocytes. Additionally, quetiapine may be beneficial for psychiatric and nonpsychiatric symptoms of MS including depression, anxiety, insomnia, and possibly even pain.
CONCLUSIONS:
These data indicate that clinical trials are justified to determine the safety, tolerability, and efficacy of Quetiapine fumarate in MS. | | Clin Pharmacokinet. 2014 May;53(5):455-65. | | Pharmacokinetics and tolerability of extended-release quetiapine fumarate in Han Chinese patients with schizophrenia.[Pubmed: 24385309] | The extended-release formulation of quetiapine (quetiapine XR), which was developed to provide more convenient once-daily administration, has been widely studied to characterize its pharmacokinetics in Caucasian populations but has rarely been studied in an Asia population. This study was conducted to evaluate the pharmacokinetics and tolerability of quetiapine XR administered as a single dose (300 mg) and multiple doses (300, 600, and 800 mg) in Han Chinese patients with schizophrenia.
METHODS AND RESULTS:
This was a single-center, open-label, single-dose and multiple-dose randomized study. Among the 55 randomized subjects, a total of 40 female or male patients in 300 mg (n = 13), 600 mg (n = 13), or 800 mg (n = 14) groups completed the study of Quetiapine fumarate XR. The treatment phase consisted of 5 consecutive days and was preceded by a 1- to 2-day titration period for the 600 and 800 mg groups. Pharmacokinetic parameters for both quetiapine and N-desalkyl quetiapine (norquetiapine) were determined. The tolerability evaluation included adverse events (AEs) noted by monitoring, physical examinations, vital signs, and clinical laboratory tests.
N-desalkyl quetiapine was formed from quetiapine with an approximate metabolite to parent ratio of 0.5 across the three dose groups. The geometric mean elimination half-life (t ½) of both quetiapine and N-desalkyl quetiapine was consistent for the three dosing groups (approximately 7 h for quetiapine and approximately 18 h for N-desalkyl quetiapine). The geometric mean maximum plasma concentrations (C max) at steady state (C max,ss) of quetiapine for the three groups were 467, 740, and 1,126 ng/mL, respectively, and for N-desalkyl quetiapine were 138, 262, and 426 ng/mL, respectively. The values for the geometric mean area under the plasma concentration-time curve over a dosing interval at the steady-state (AUCss) of quetiapine were 5,094, 7,685, and 13,237 ng·h/mL, respectively, and for N-desalkyl quetiapine were 2,284, 4,341, and 7,216 ng·h/mL, respectively. The apparent oral clearance (CL/F) of quetiapine at steady state appeared to be comparable across the three dose groups. The pharmacokinetics of quetiapine XR were dose-proportional across the dosage range employed. The most common AE was somnolence, but all of the reported AEs were mild. There were no serious AEs or other significant AEs.
CONCLUSIONS:
Quetiapine fumarate XR has a dose-proportional pharmacokinetic profile at doses ranging from 300 to 800 mg once daily, and a slower time to reach C max and steady state after 3 days of sequential dosing. Therefore, it offers a simple and rapid dose-escalation option and more convenient once-daily administration. The three dosages of Quetiapine fumarate XR were generally well-tolerated in this pharmacokinetic study of Han Chinese patients with schizophrenia. | | J Clin Psychiatry. 2009 Apr;70(4):526-39. | | Extended release quetiapine fumarate monotherapy in major depressive disorder: a placebo- and duloxetine-controlled study.[Pubmed: 19358790] | To evaluate the efficacy and tolerability of once-daily extended release Quetiapine fumarate (quetiapine XR) as monotherapy treatment for major depressive disorder (MDD).
METHODS AND RESULTS:
This 8-week (6-week active-treatment, randomized phase; 2-week posttreatment drug-discontinuation/tapering phase), multicenter, double-blind, randomized, parallel-group, placebo- and active-controlled, phase 3 study was conducted between April 2006 and May 2007. In total, 612 patients with Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)-defined MDD were randomly assigned to quetiapine XR 150 mg/day or 300 mg/day, duloxetine 60 mg/day (active control), or placebo. The primary endpoint was the change from baseline to week 6 in Montgomery-Asberg Depression Rating Scale (MADRS) total score.
CONCLUSIONS:
Quetiapine XR monotherapy (150 mg/day and 300 mg/day) is effective, with safety and tolerability consistent with the known profile of quetiapine XR, in the treatment of patients with MDD, with onset of symptom improvement demonstrated at week 1. | | Psychopharmacol Bull. 2008;41(3):11-35. | | The efficacy and tolerability of once-daily extended release quetiapine fumarate in hospitalized patients with acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled study.[Pubmed: 18779774] | This study aimed to demonstrate efficacy of once-daily extended release Quetiapine fumarate (quetiapine XR) versus placebo in patients with acute schizophrenia.
METHODS AND RESULTS:
In this 6-week, randomized, double-blind study (5077IL/0041) patients were randomized to receive quetiapine XR (300, 600, or 800 mg/day), Quetiapine fumarate immediate release (quetiapine IR) [300 or 600 mg/day], or placebo. Primary endpoint was change from baseline in the Positive and Negative Syndrome Scale (PANSS) total score at Day 42. Secondary variables included PANSS response rate at Day 42 (>/=30% decrease in PANSS total score from baseline) and Clinical Global Impressions Severity (CGI-S) and Improvement (CGI-I) ratings. Safety assessments included adverse event (AE) reporting and laboratory measures. Of 532 patients randomized, 222 (41.7%) completed the study. Improvements in PANSS total scores from baseline to Day 42 across treatment groups were: quetiapine XR 300 mg/day -5.01, 600 mg/day -13.01 and 800 mg/day -11.17, quetiapine IR 300 mg/day -9.42 and 600 mg/day -6.97, and placebo -5.19; the difference in change was statistically significant only for quetiapine XR 600 mg/day (p = 0.033). There were no statistically significant differences between active treatment groups and placebo for PANSS response rates. Several post hoc analyses were conducted to explain the study efficacy outcome but these were inconclusive. Quetiapine XR was generally well tolerated with the majority of AEs being mild or moderate in intensity and no unexpected AEs.
CONCLUSIONS:
Superior efficacy of quetiapine XR versus placebo in patients with schizophrenia was demonstrated for quetiapine XR 600 mg/day. The safety and tolerability profile of quetiapine XR was similar to that of quetiapine IR. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)