| In vivo: |
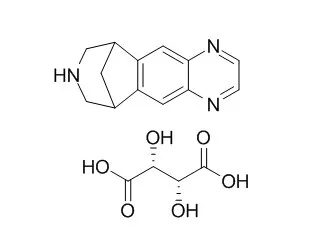
| Nicotine Tob Res. 2014 Nov;16(11):1495-502. | | Safety of varenicline tartrate and counseling versus counseling alone for smoking cessation: a randomized controlled trial for inpatients (STOP study).[Pubmed: 25031315] | Inpatient medical settings offer an opportunistic environment for initiating smoking cessation interventions to patients reflecting on their health. Current evidence has shown the superior efficacy of Varenicline tartrate (VT) for smoking cessation compared with other tobacco cessation therapies; however, recent evidence also has highlighted concerns about the safety and tolerability of Varenicline tartrate. Given these apprehensions, we aimed to evaluate the safety and effectiveness of Varenicline tartrate plus quitline-counseling compared to quitline-counseling alone in the inpatient medical setting.
METHODS AND RESULTS:
Adult patients (n = 392, 20-75 years) admitted with a smoking-related illnesses to 3 hospitals were randomized to receive either 12 weeks of Varenicline tartrate (titrated from 0.5mg daily to 1mg twice daily) plus quitline-counseling (VT+C), (n = 196) or quitline-counseling alone (n = 196). Varenicline tartrate was well tolerated in the inpatient setting among subjects admitted with acute smoking-related illnesses (mean age 52.8±2.89 and 53.7±2.77 years in the Varenicline tartrate+C and counseling alone groups, respectively). The most common self-reported adverse event during the 12-week treatment phase was nausea (16.3% in the Varenicline tartrate+C group compared with 1.5% in the counseling alone group). Thirteen deaths occurred during the study period (n = 6 were in the Varenicline tartrate+C arm compared with n = 7 in the counseling alone arm). All of these subjects had known comorbidities or developed underlying comorbidities.
CONCLUSIONS:
Varenicline tartrate appears to be a safe and well-tolerated opportunistic treatment for inpatient smokers who have related chronic disease. Based on the proven efficacy of varenicline from outpatient studies and our recent inpatient evidence, we suggest it be considered as part of standard care in the hospital setting. | | J Addict Med. 2013 Jul-Aug;7(4):277-86. | | A double-blind, placebo-controlled trial assessing the efficacy of varenicline tartrate for alcohol dependence.[Pubmed: 23728065] | To assess the efficacy and safety of Varenicline tartrate (Chantix) for the treatment of alcohol dependence. Varenicline tartrate is a partial α4β2 nicotinic acetylcholine agonist approved by the Food and Drug Administration for smoking cessation. It has reduced drinking in animal studies and in small studies of humans who were both heavy drinkers and smokers. This is the first multisite clinical trial of varenicline in a population of smokers and nonsmokers with alcohol dependence.
METHODS AND RESULTS:
Men and women (n = 200) meeting the criteria for alcohol dependence were recruited across 5 clinical sites. Patients received double-blind varenicline or placebo and a computerized behavioral intervention. Varenicline tartrate was titrated during the first week to 2 mg/d, which was maintained during weeks 2 to 13. The Varenicline tartrate group had significantly lower weekly percent heavy drinking days (primary outcome) (adjusted mean difference = 10.4), drinks per day, drinks per drinking day, and alcohol craving compared with the placebo group (P < 0.05). The average treatment effect on alcohol use was similar for smokers and nonsmokers. Varenicline tartrate was well-tolerated; adverse events were expected and mild.
CONCLUSIONS:
Varenicline tartrate significantly reduced alcohol consumption and craving, making it a potentially viable option for the treatment of alcohol dependence. | | AIDS Patient Care STDS. 2012 Jan;26(1):12-9. | | Safety and tolerability of varenicline tartrate (Champix(®)/Chantix(®)) for smoking cessation in HIV-infected subjects: a pilot open-label study.[Pubmed: 22007690] | The prevalence of smoking in HIV-infected subjects is high. As a smoking cessation aid, Varenicline tartrate (Champix(®), Pfizer, Saint-Laurent, QC, Canada or Chantix(®), Pfizer, Mission, KS) has not been previously evaluated in HIV-infected smokers.
METHODS AND RESULTS:
In this multicenter pilot open label study, Varenicline tartrate 1.0 mg was used twice daily for 12 weeks with dose titration in the first week. Adverse events (AEs) during the treatment period were recorded. Changes from baseline in laboratory tests, vital signs, daily cigarette consumption, nicotine dependence, and withdrawal were measured through week 24. Self-reported abstinence was validated by serum cotinine at week 12. We enrolled 36 subjects with a mean of 29 pack-years of smoking and a minimum of 4 cigarettes per day. All but 1 were male, 33 (92%) were white. The most frequently reported AEs were nausea (33%), abnormal dreams (31%), affect lability (19%), and insomnia (19%). Six (17%) subjects discontinued Varenicline tartrate due to AEs. No grade 3/4 laboratory abnormalities or serious AEs occurred during the study. There was no significant change in HIV viral load. CD4 counts increased by 69 cells/mm3 (p = 0.001) at week 24. Serum cotinine-verified 4-week continuous abstinence rate through weeks 9-12 was 42% (95% confidence interval [CI]: 26-58%). AEs and abstinence rates were comparable to those in published randomized controlled trials conducted in generally healthy HIV-negative smokers.
CONCLUSIONS:
Varenicline tartrate was safe and appears effective among HIV-infected smokers in this exploratory study, although AEs were common. The most common AE was nausea, with no adverse effect on HIV treatment outcome. Close monitoring of liver enzymes and blood pressure is recommended for HIV-positive smokers taking varenicline. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)