| In vitro: |
| Epidemiol Infect . 1992 Apr;108(2):271-278. | | Apramycin resistance plasmids in Escherichia coli: possible transfer to Salmonella typhimurium in calves[Pubmed: 1582469] | | An outbreak of salmonellosis in calves was monitored for persistence of Salmonella typhimurium excretion in faeces and the effect of treatment with apramycin. Prior to treatment apramycin-resistant Escherichia coli were present but all S. typhimurium isolates were sensitive. Following the treatment of six calves with apramycin, apramycin-resistant S. typhimurium were isolated from two treated calves and one untreated calf. Plasmid profiles of E. coli and S. typhimurium were compared and plasmids conferring resistance to apramycin and several other antibiotics were transferred by conjugation in vitro from calf E. coli and S. typhimurium isolates to E. coli K-12 and from E. coli to S. typhimurium. The plasmids conjugated with high frequency in vitro from E. coli to S. typhimurium, and hybridized to a DNA probe specific for the gene encoding aminoglycoside acetyltransferase 3-IV (AAC(3)-IV) which confers resistance to apramycin, gentamicin, netilmicin and tobramycin. | | J Bacteriol . 1996 Nov;178(21):6357-6360. | | Apramycin resistance as a selective marker for gene transfer in mycobacteria[Pubmed: 8892841] | | We have explored the potential of using the apramycin resistance gene as a marker in mycobacterial gene transfer studies. Shuttle plasmids available for both electroporation and conjugation studies have been constructed, and we have successfully validated the use of the apramycin resistance gene as a component of cloning vectors for Mycobacterium smegmatis, M. bovis BCG, and M. tuberculosis. | | J Antimicrob Chemother . 2006 Jul;58(1):101-107. | | Correlation between apramycin and gentamicin use in pigs and an increasing reservoir of gentamicin-resistant Escherichia coli[Pubmed: 16709594] | | Objectives: Resistance towards the veterinary drug apramycin can be caused by the aac(3)-IV gene, which also confers resistance towards the important human antibiotic gentamicin. The objectives of this study were to investigate the temporal occurrence and the genetic background of apramycin and gentamicin resistance in Escherichia coli strains from pork, healthy pigs and diagnostic submissions from pigs and to investigate potential relationships to the use of apramycin and gentamicin at farm and national levels.
Methods: Data on Danish E. coli isolates from healthy pigs (indicator bacteria), diagnostic submissions from pigs (clinical isolates) and pork were obtained from the national surveillance of antimicrobial resistance and from routine diagnostic laboratories. Antimicrobial consumption data were obtained from the Danish Medicines Agency (1997-2000) and from the VetStat database (2001-2004). The genetic background for gentamicin resistance was investigated by PCR. Relationships between antimicrobial usage and resistance were analysed by chi2 test and logistic regression.
Results: At the farm level, the occurrence of apramycin/gentamicin cross-resistance was correlated to the use of apramycin (P < 0.001). At the national level, occurrence of apramycin/gentamicin cross-resistance in clinical E. coli O149 isolates was significantly correlated with the amounts and duration of apramycin use. The aac(3)-IV gene was detected in all tested cross-resistant isolates.
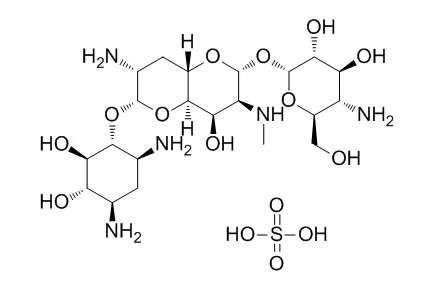
Conclusions: Apramycin consumption at farm level is most probably driving the increasing occurrence of apramycin/gentamicin cross-resistant [aac(3)-IV positive] E. coli in diseased pigs and healthy finishers at slaughter. The duration of use and amounts used both had a significant effect on the prevalence of apramycin/gentamicin cross-resistance in diseased weaning pigs at the national level. | | Int J Antimicrob Agents . 1999 Aug;12(3):229-237. | | Postantibiotic and physiological effects of tilmicosin, tylosin, and apramycin at subminimal and suprainhibitory concentrations on some swine and bovine respiratory tract pathogens[Pubmed: 10461841] | | The antimicrobial activity of tilmicosin, tylosin, and apramycin on some important gram-negative swine and bovine pathogens namely, Pasteurella multocida, Pasteurella haemolytica, Bordetella bronchiseptica, and Actinobacillus pleuropneumoniae were studied in vitro. The effect of minimal inhibitory concentrations (MICs) and sub-MICs (1/4, 1/2 MIC) on bacterial growth was evaluated. The presence of tilmicosin, tylosin and apramycin in the medium decreased the rate of growth of the bacterial strains tested using drug concentrations as low as 1/4 MIC. The postantibiotic effect (PAE) which is the suppression of optimal bacterial growth that persists after a short exposure (2 h) of microorganisms to an antibiotic was studied by exposure of bacteria to drugs at 1/4, 1/2, 1, 4 and 8 times MIC. The duration of PAEs increased with rising concentration for all drugs tested but at concentrations below the MIC, tilmicosin showed more significant PAEs than tylosin or apramycin against P. multocida and A. pleuropneumoniae. Tilmicosin and tylosin caused PAEs of up to 8 h when used at 8 times the MIC, while apramycin caused PAEs of up to 5 h when used at this concentration. Sub-MICs of either tilmicosin, tylosin, or apramycin had no effect on P. multocida dermonecrotic toxin production. However sub-MICs of tylosin, or apramycin significantly reduced the haemolytic activity of A. pleuropneumoniae and affected the capsular material production of this isolate and of one isolate of P. multocida (type A). The in vitro effect of tilmicosin, tylosin, and apramycin (even when used at sub-MIC levels) on growth, production of capsular material, and haemolytic activity might impair the virulence of some of the microorganisms studied. In addition to the effects of these drugs on some putative virulence factors, we suggest that the strong PAEs caused by tilmicosin, tylosin, and apramycin may also contribute to the in vivo efficacy of these drugs. | | mBio . 2021 Feb 9;12(1):e02705-20. | | ApmA Is a Unique Aminoglycoside Antibiotic Acetyltransferase That Inactivates Apramycin[Pubmed: 33563840] | | Apramycin is an aminoglycoside antibiotic with the potential to be developed to combat multidrug-resistant pathogens. Its unique structure evades the clinically widespread mechanisms of aminoglycoside resistance that currently compromise the efficacy of other members in this drug class. Of the aminoglycoside-modifying enzymes that chemically alter these antibiotics, only AAC(3)-IVa has been demonstrated to confer resistance to apramycin through N-acetylation. Knowledge of other modification mechanisms is important to successfully develop apramycin for clinical use. Here, we show that ApmA is structurally unique among the previously described aminoglycoside-modifying enzymes and capable of conferring a high level of resistance to apramycin. In vitro experiments indicated ApmA to be an N-acetyltransferase, but in contrast to AAC(3)-IVa, ApmA has a unique regiospecificity of the acetyl transfer to the N2' position of apramycin. Crystallographic analysis of ApmA conclusively showed that this enzyme is an acetyltransferase from the left-handed β-helix protein superfamily (LβH) with a conserved active site architecture. The success of apramycin will be dependent on consideration of the impact of this potential form of clinical resistance.IMPORTANCE Apramycin is an aminoglycoside antibiotic that has been traditionally used in veterinary medicine. Recently, it has become an attractive candidate to repurpose in the fight against multidrug-resistant pathogens prioritized by the World Health Organization. Its atypical structure circumvents most of the clinically relevant mechanisms of resistance that impact this class of antibiotics. Prior to repurposing apramycin, it is important to understand the resistance mechanisms that could be a liability. Our study characterizes the most recently identified apramycin resistance element, apmA We show ApmA does not belong to the protein families typically associated with aminoglycoside resistance and is responsible for modifying a different site on the molecule. The data presented will be critical in the development of apramycin derivatives that will evade apmA in the event it becomes prevalent in the clinic. | | Microb Drug Resist . 2020 May 14. | | Investigation of the In Vitro Effectiveness of Aztreonam/Avibactam, Colistin/Apramycin, and Meropenem/Apramycin Combinations Against Carbapenemase-Producing, Extensively Drug-Resistant Klebsiella pneumoniae Strains[Pubmed: 32401692] | | This study aimed at investigating the in vitro effectiveness of aztreonam/avibactam, colistin/avibactam, colistin/apramycin, and meropenem/apramycin combinations against carbapenemase-producing, extensively drug-resistant (XDR) Klebsiella pneumoniae strains. This study evaluated 38 carbapenem-resistant, carbapenemase-producing, and XDR K. pneumoniae strains. The checkerboard method was used to examine the efficacy of aztreonam/avibactam, and meropenem/apramycin combinations in all strains and the colistin/apramycin combination in colistin-resistant strains (n = 26). It was found that when used alone, aztreonam and avibactam had high minimum inhibitory concentration values in all strains and that all strains were resistant to aztreonam. Nevertheless, the aztreonam/avibactam combination was found to have a synergistic effect against all strains. Apramycin alone was effective against 30 K. pneumoniae strains (79%); however, 8 strains (21%) were found to be resistant. In the synergy testing of 26 colistin-resistant strains with the checkerboard method, the colistin/apramycin combination was found to have a synergistic effect against 4 strains (15.3%), an antagonistic effect against 8 strains (30.7%), and an additive effect against 14 strains (54%). By comparison, the meropenem/apramycin combination had a synergistic effect against 20 strains (52%) and an additive effect against 12 strains (31%). The aztreonam/avibactam combination showed a high in vitro synergistic effect on carbapenemase-producing and XDR K. pneumoniae strains, such as Metallo-β-lactamase, and provided good prospects for the successful treatment. The meropenem/apramycin combination was also highly synergistic. The synergistic effects were low for the colistin/apramycin combination that was tested on colistin-resistant strains. However, it is promising that apramycin has low minimal inhibitory concentration values. |
|
| In vivo: |
| Avian Pathol. 1987;16(2):319-326. | | Evaluation of the efficacy of apramycin against Salmonella pullorum infection in chickens[Pubmed: 18766617] | | The efficacy of apramycin given orally at dose levels of 225, 150 and 75 mg/litre for five days to chicks experimentally infected with Salmonella pullorum has been evaluated. The results show that this drug, when utilised at the dose level of 225 mg/litre for five days, totally suppresses mortality and significantly reduces Salmonella excretion in comparison with non-treated chicks. | | Antimicrob Agents Chemother . 2022 Feb 15;66(2):e0151021. | | Apramycin Overcomes the Inherent Lack of Antimicrobial Bactericidal Activity in Mycobacterium abscessus[Pubmed: 34930031] | | Antibiotic therapy of infections caused by the emerging pathogen Mycobacterium abscessus is challenging due to the organism's inherent resistance to clinically available antimicrobials. The low bactericidal potency of currently available treatment regimens is of concern and testifies to the poor therapeutic outcomes for pulmonary M. abscessus infections. Mechanistically, we demonstrate here that the acetyltransferase Eis2 is responsible for the lack of bactericidal activity of amikacin, the standard aminoglycoside used in combination treatment. In contrast, the aminoglycoside apramycin, with a distinct structure, is not modified by any of the pathogen's innate aminoglycoside resistance mechanisms and is not affected by the multidrug resistance regulator WhiB7. As a consequence, apramycin uniquely shows potent bactericidal activity against M. abscessus. This favorable feature of apramycin is reflected in a mouse model of pulmonary M. abscessus infection, which demonstrates superior activity, compared with amikacin. These findings encourage the development of apramycin for the treatment of M. abscessus infections and suggest that M. abscessus eradication in pulmonary disease may be within therapeutic reach. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)