| In vitro: |
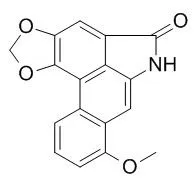
| Toxicol In Vitro. 2010 Jun;24(4):1092-7. | | Toxicities of aristolochic acid I and aristololactam I in cultured renal epithelial cells.[Pubmed: 20338233] | Aristolochic acid nephropathy, a progressive tubulointerstitial renal disease, is primarily caused by aristolochic acid I (AA-I) intoxication. Aristololactam I (AL-I), the main metabolite of AA-I, may also participate in the processes that lead to renal damage.
METHODS AND RESULTS:
To investigate the role and mechanism of the Aristololactam I -mediated cytotoxicity, we determined and compared the cytotoxic effects of AA-I and Aristololactam I on cells of the human proximal tubular epithelial (HK-2) cell line. To this end, we treated HK-2 cells with AA-I and Aristololactam I and assessed the cytotoxicity of these agents by using the 3-(4,5-dimethyl-thiazol-2-yl)-2,5-diphenyl-tetrazolium bromide (MTT) assay, flow cytometry, and an assay to determine the activity of caspase 3. The proliferation of HK-2 cells was inhibited in a concentration- and time-dependent manner. Cell-cycle analysis revealed that the cells were arrested in the S-phase. Apoptosis was evidenced by the results of the annexin V/propidium iodide (PI) assay and the occurrence of a sub-G1 peak. In addition, AA-I and AL-I increased caspase 3-like activity in a concentration-dependent manner.
CONCLUSIONS:
These results also suggested that the cytotoxic potency of Aristololactam I is higher than that of AA-I and that the cytotoxic effects of these molecules are mediated through the induction of apoptosis in a caspase 3-dependent pathway. | | Zhongguo Zhong Yao Za Zhi. 2004 Jan;29(1):78-83. | | Injury in renal proximal tubular epithelial cells induced by aristololactam I.[Pubmed: 15709390] | To study whether Aristololactam I (AL-I) induces injury in human renal proximal tubular epithelial cells.
METHODS AND RESULTS:
Cultured human renal proximal tubular epithelial cell line HK-2 was used as the subject. Aristolochic Acid I (AA-I) was used as a positive control. Cell toxicity of Aristololactam I was detected by LDH releasing rate. Cell apoptosis was evaluated by cellular morphology, DNA content and expression of cell membrane phosphatidylserine (PS). The secretion level of fibronectin (FN) and TGF-beta1 in HK-2 cells were assayed by ELISA. Aristololactam I had a direct toxicity on HK-2 in a dose dependent manner from 2.5 mg x mL(-1) to 20 mg x mL(-1); In these range of concentration, Aristololactam I could induce cell apoptosis which was detectable by measurements of morphology, DNA content and expression of PS. Aristololactam I could stimulate the secretion of FN and TGF-beta1. The potency of Aristololactam I cell toxicity was higher than AA-I at the same concentration. The effects of Aristololactam I on apoptosis, secretion of FN and TGF-beta1 were all weaker than AA-I.
CONCLUSIONS:
Aristololactam I as one metabolite of AA-I in vivo induces direct injury in renal proximal tubular cells. Its effects are similar to those of AA-I. Aristololactam I may be one of toxic metabolites in Chinese herbs containing AA which participate in renal damage and fibrosis. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)