| Description: |
Kaerophyllin has anti-fibrotic effects, it can protect the rat liver from TAA-caused injury and fibrogenesis by suppressing hepatic inflammation and inhibiting HSC activation, possibly through upregulation of PPAR-γ expression. Kaerophyllin inhibits AB-induced LX-2 activation and migration with downregulation of Akt/ERK phosphorylations and NF-κB activity. |
| Targets: |
TNF-α | PPAR | Akt | ERK | NF-kB | IL Receptor |
| In vitro: |
| Liver Int. 2011 May;31(5):618-29. | | Kaerophyllin inhibits hepatic stellate cell activation by apoptotic bodies from hepatocytes.[Pubmed: 21457435] | Hepatic stellate cells (HSCs), the key cell type for hepatic fibrosis, become activated and profibrogenic in the presence of hepatocyte apoptotic bodies (ABs). Bupleurum scorzonerifolium (BS), a widely used traditional Chinese herb for liver diseases, was fractionated, and the inhibitory effects of BS extracts on AB-induced HSC migration were screened. The activity-guided fractionation led to a lignan, Kaerophyllin. In this study, the anti-fibrotic effects of Kaerophyllin were studied in the presence of ABs.
METHODS AND RESULTS:
LX-2 cells phagocytosing ultraviolet (UV)-induced HepG2 ABs were investigated by confocal microscopy and flow cytometry. AB-induced HSC activation was evaluated by immunoblotting and real-time PCR analyses. HSC migration was measured by wound-healing assays. HepG2 ABs induced LX-2 activation, with the production of collagen I and α-smooth muscle actin, upregulated profibrogenic gene transcriptions and increased NF-κB activity, cell migration and phagocytosis. Kaerophyllin from BS antagonized AB-induced HSC migration and activation.
CONCLUSIONS:
Kaerophyllin inhibited AB-induced LX-2 activation and migration with downregulation of Akt/ERK phosphorylations and NF-κB activity. Our study suggests a novel platform for screening anti-fibrotic compounds with ABs. |
|
| In vivo: |
| Planta Med. 2011, 77(12):1410-1410. | | Kaerophyllin Suppresses Hepatic Stellate Cell Activation by Apoptotic Bodies and Ameliorates Hepatic Fibrosis in Rats.[Reference: WebLink] | Hepatocyte apoptosis is a central feature of many liver diseases, leading to liver inflammation and fibrosis. In this study, we screened potential drugs inhibiting hepatic stellate cell (HSC) migration induced by hepatocyte apoptotic bodies (ABs) and evaluated the in vivo therapeutic effects in a rat model of hepatic fibrosis induced by thioacetamide (TAA).
METHODS AND RESULTS:
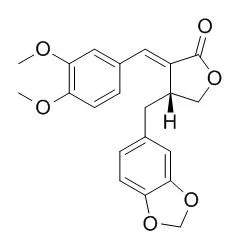
Rat HSCs were exposed to UV-irradiated hepatocyte ABs or TNF-α to investigate the anti-fibrotic effects of Kaerophyllin. Liver fibrosis was induced by TAA injection into rats twice weekly for 6 weeks. Kaerophyllin (10 or 30mg/kg) or curcumin (150mg/kg, as a positive control) was given by gavage twice daily for 4 weeks starting 2 weeks after TAA injection. Kaerophyllin (α-(trans-3,4-dimethoxybenzylidene)-β-(3,4-methylenedioxy-benzyl)-γ-butyrolactone, a lignan isolated from a Chinese herb Bupleurum scorzonerifolium by bioactivity-guided fractionation) attenuated ABs- and TNF-α-induced HSC migration, protein levels of collagen I and α-SMA, and the mRNA levels of ICAM-1, MCP-1 and IL-1β genes, but elevated PPAR-γ luciferase activity. Furthermore, Kaerophyllin reduced TNF-α- and ABs-induced NF-κB luciferase activity with decreased IκB phosphorylation and p65 nuclear translocation. In TAA rats, Kaerophyllin and curcumin treatment significantly protected liver from injury by reducing serum AST and ALT levels, and improved the histological architecture and fibrosis score. In addition, Kaerophyllin treatment suppressed α-SMA protein expression, and mRNA levels of collagen I, TIMP-1, TNF-α, IL-1β and MCP-1 genes in TAA rats.
CONCLUSIONS:
Our results demonstrated that Kaerophyllin protected the rat liver from TAA-caused injury and fibrogenesis by suppressing hepatic inflammation and inhibiting HSC activation. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)