| In vitro: |
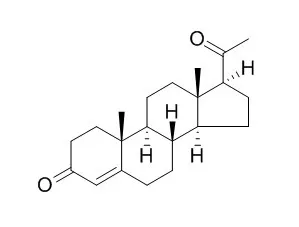
| J Endocrinol. 2015 Feb;224(2):183-94. | | Progesterone-induced activation of membrane-bound progesterone receptors in murine macrophage cells.[Pubmed: 25472814 ] | Parturition is an inflammatory process mediated to a significant extent by macrophages. Progesterone (P4) maintains uterine quiescence in pregnancy, and a proposed functional withdrawal of P4 classically regulated by nuclear Progesterone receptors (nPRs) leads to labor. P4 can affect the functions of macrophages despite the reported lack of expression of nPRs in these immune cells.
METHODS AND RESULTS:
Therefore, in this study we investigated the effects of the activation of the putative membrane-associated PR on the function of macrophages (a key cell for parturition) and discuss the implications of these findings for pregnancy and parturition. In murine macrophage cells (RAW 264.7), activation of mPRs by P4 modified to be active only extracellularly by conjugation to BSA (P4BSA, 1.0×10(-7) mol/l) caused a pro-inflammatory shift in the mRNA expression profile, with significant upregulation of the expression of cyclooxygenase 2 (COX2 (Ptgs2)), Il1B, and Tnf and downregulation of membrane Progesterone receptor alpha (Paqr7) and oxytocin receptor (Oxtr). Pretreatment with PD98059, a MEK1/2 inhibitor, significantly reduced P4BSA-induced expression of mRNA of Il1B, Tnf, and Ptgs2. Inhibition of protein kinase A (PKA) by H89 blocked P4BSA-induced expression of Il1B and Tnf mRNA. P4BSA induced rapid phosphorylation of MEK1/2 and CREB (a downstream target of PKA). This phosphorylation was inhibited by pretreatment with PD98059 and H89, respectively, revealing that MEK1/2 and PKA are two of the components involved in mPR signaling.
CONCLUSIONS:
Taken together, these results indicate that changes in membrane Progesterone receptor alpha expression and signaling in macrophages are associated with the inflammatory responses; and that these changes might contribute to the functional withdrawal of P4 related to labor. |
|
| In vivo: |
| J Steroid Biochem Mol Biol. 2015 Mar;147:31-9. | | Progesterone-induced down-regulation of hormone sensitive lipase (Lipe) and up-regulation of G0/G1 switch 2 (G0s2) genes expression in inguinal adipose tissue of female rats is reflected by diminished rate of lipolysis.[Pubmed: 25448749] | Decreased lipolytic activity in adipose tissue may be one of the reasons behind excess accumulation of body fat during pregnancy.
METHODS AND RESULTS:
The aim of this study was to analyze the effect of Progesterone on the expression of: (a) Lipe (encoding hormone-sensitive lipase, HSL), (b) Pnpla2 (encoding adipose triglyceride lipase, ATGL), (c) abhydrolase domain containing 5 (Abhd5), and (d) G0/G1 switch 2 (G0s2) genes in white adipose tissue (WAT), as potential targets for Progesterone action during the course of pregnancy. Administration of Progesterone to female rats, which was reflected by approximately 2.5-fold increase in circulating Progesterone concentration, is associated with a decrease in Lipe gene expression in the inguinal WAT. The expression of Pnpla2 gene in all main fat depots of females and males remained unchanged after Progesterone administration. Administration of Progesterone resulted in an increase in the expression of Abhd5 gene (whose product increases ATGL activity) and G0s2 gene (whose product decreases ATGL activity) in the inguinal WAT of female rats. Mifepristone, a selective antagonist of Progesterone receptor, abolished the effect of Progesterone on Lipe, Abhd5 and G0s2 genes expression in the inguinal WAT. The decrease in Lipe and the increase in Abhd5 and G0s2 genes expression was associated with lower rate of stimulated lipolysis. Administration of Progesterone exerted no effect on Lipe, Abhd5 and G0s2 genes expression and stimulated lipolysis in the retroperitoneal WAT of females, as well as in the inguinal, epididymal and retroperitoneal WAT of males.
CONCLUSIONS:
In conclusion, our findings suggest that Progesterone decreases the rate of lipolysis in the inguinal WAT of female rats, inhibiting the activity of both ATGL (by stimulating synthesis of G0S2 - specific inhibitor of the enzyme) and HSL (due to inhibition of Lipe gene expression). | | Am J Obstet Gynecol. 2015 Mar;212(3):335.e1-7. | | Effects of exogenous progesterone on fetal nuchal translucency: an observational prospective study.[Pubmed: 25305408] | Nuchal translucency (NT) seen ultrasonographically at 11-14 weeks' gestation is a sensitive marker for Down syndrome. Despite its important role for Down syndrome screening, its use is still considered controversial due to high false-positive rates. We speculated that Progesterone could lead to abnormal blood flow patterns and, subsequently, to increased NT. Our primary endpoint was to evaluate the effects of exogenous Progesterone on NT thickness compared to controls. The secondary endpoint was to evaluate these effects in a subgroup at low risk for fetal aneuploidies, identifying the strongest factors influencing NT variation. The tertiary endpoint was to evaluate, within the treatment group, if there is any difference in NT according to the type of Progesterone administered, route of administration, and dose regimen.
METHODS AND RESULTS:
All women who came to measure NT at 11-14 weeks' gestation (crown-rump length between 45-84 mm) were considered eligible. We divided patients into 2 groups: women receiving exogenous Progesterone and controls. Afterwards, 3 NT scans were performed for each case, and the largest value, accurate to 2 decimal points, was recorded.
In all, 3716 women were enrolled and analyzed. In a crude analysis, NT (P < .05) increased in the exogenous Progesterone group. The same results were obtained in the low-risk group (P < .05). The factorial analysis of variance model confirmed a correlation between altered NT and gestational age (P < .0001) and Progesterone exposure (P < .05). The characteristics of treatment (route, formulation, dose) were examined separately and no statistically significant differences among the subgroups were observed.
CONCLUSIONS:
Exogenous Progesterone increases NT. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)