| Kinase Assay: |
| Metabolism. 2015 Mar;64(3):428-37. | | Mangiferin inhibits endoplasmic reticulum stress-associated thioredoxin-interacting protein/NLRP3 inflammasome activation with regulation of AMPK in endothelial cells.[Pubmed: 25499441] |
METHODS AND RESULTS:
Mangiferin effectively inhibited ER stress-associated oxidative stress by attenuating IRE1α phosphorylation and reducing ROS production. In response to ER stress, thioredoxin-interacting protein (TXNIP) expression increased, followed by NLRP3 inflammasome activation and increased IL-1β secretion. Mangiferin treatment attenuated the expressions of TXNIP and NLRP3 and reduced IL-1β and IL-6 production, demonstrating its inhibitory effects on TXNIP/NLRP3 inflammasome activation. NLRP3 inflammasome activation is responsible for mitochondrial cell death. Mangiferin restored the loss of the mitochondrial membrane potential (Δψm) and inhibited caspase-3 activity, and thereby protected cells from high glucose-induced apoptosis. Moreover, Mangiferin inhibited ET-1 secretion and restored the loss of NO production when cells were exposed to high glucose. Mangiferin enhanced AMPK phosphorylation and AMPK inhibitor compound C diminished its beneficial effects, indicating the potential role of AMPK in its action.
CONCLUSIONS:
Our work showed the beneficial effects of Mangiferin on the improvement of endothelial homeostasis and elucidated the molecular pathway through which Mangiferin ameliorated endothelial dysfunction by inhibition of ER stress-associated TXNIP/NLRP3 inflammasome activation in endothelial cells.These findings demonstrated the beneficial effects of Mangiferin on the regulation of endothelial homeostasis and indicated its potential application in the management of diabetic cardiovascular complications. | | J Cell Biochem. 2011 Jan;112(1):89-97. | | Mangiferin attenuates osteoclastogenesis, bone resorption, and RANKL-induced activation of NF-κB and ERK.[Pubmed: 20683903 ] | Osteolytic bone diseases such as osteoporosis have a common pathological feature in which osteoclastic bone resorption outstrips bone synthesis. Osteoclast formation and activation are regulated by receptor activator of nuclear factor κB ligand (RANKL). The induction of RANKL-signaling pathways occurs following the interaction of RANKL to its cognate receptor, RANK. This specific binding drives the activation of downstream signaling pathways; which ultimately induce the formation and activation of osteoclasts.
METHODS AND RESULTS:
In this study, we showed that a natural immunomodulator, Mangiferin, inhibits osteoclast formation and bone resorption by attenuating RANKL-induced signaling. Mangiferin diminished the expression of osteoclast marker genes, including cathepsin K, calcitonin receptor, DC-STAMP, and V-ATPase d2. Mechanistic studies revealed that Mangiferin inhibits RANKL-induced activation of NF-κB, concomitant with the inhibition of IκB-α degradation, and p65 nuclear translocation. In addition, Mangiferin also exhibited an inhibitory effect on RANKL-induced ERK phosphorylation.
CONCLUSIONS:
Collectively, our data demonstrates that Mangiferin exhibits anti-resorptive properties, suggesting the potential application of Mangiferin for the treatment and prevention of bone diseases involving excessive osteoclastic bone resorption. |
|
| Cell Research: |
| Genet Mol Res. 2015 May 12;14(2):4989-5002. | | Mangiferin induces cell cycle arrest at G2/M phase through ATR-Chk1 pathway in HL-60 leukemia cells.[Pubmed: 25966274] | This study aimed to determine the effect of Mangiferin on the cell cycle in HL-60 leukemia cells and expression of the cell cycle-regulatory genes Wee1, Chk1 and CDC25C and to further investigate the molecular mechanisms of the antileukemic action of Mangiferin.
METHODS AND RESULTS:
The inhibitory effect of Mangiferin on HL-60 leukemia cell proliferation was determined by the MTT assay. The impact of Mangiferin on the HL-60 cell cycle was evaluated by flow cytometry. After the cells were treated with different concentrations of Mangiferin, the expression levels of Wee1, Chk1 and CDC25C mRNA were determined by RT-PCR, and Western blot was used to evaluate the expression levels of cdc25c, cyclin B1, and Akt proteins. The inhibition of HL-60 cell growth by Mangiferin was dose- and time-dependent. After treatment for 24 h, cells in G2/M phase increased, and G2/M phase arrest appeared with increased mRNA expression of Wee1, Chk1 and CDC25C. Mangiferin inhibited Chk1 and cdc25c mRNA expression at high concentrations and induced Wee1 mRNA expression in a dose-dependent manner. It significantly inhibited ATR, Chk1, Wee1, Akt, and ERK1/2 phosphorylation but increased cdc2 and cyclin B1 phosphorylation. Furthermore, Mangiferin reduced cdc25c, cyclin B1, and Akt protein levels while inducing Wee1 protein expression. It also antagonized the phosphorylation effect of vanadate on ATR, and the phosphorylation effect of EGF on Wee1.
CONCLUSIONS:
These findings indicated that Mangiferin inhibits cell cycle progression through the ATR-Chk1 stress response DNA damage pathway, leading to cell cycle arrest at G2/M phase in leukemia cells. |
|
| Animal Research: |
| Phytother Res. 2015 Feb;29(2):295-302. | | Mangiferin attenuates renal fibrosis through down-regulation of osteopontin in diabetic rats.[Pubmed: 25380391] | This study was designed to investigate the effects of Mangiferin on renal fibrosis, osteopontin production, and inflammation in the kidney of diabetic rats.
METHODS AND RESULTS:
Diabetes was induced through the single administration of streptozotocin (55 mg/kg, i.p.). Diabetic rats were treated with Mangiferin (15, 30, and 60 mg/kg/day, i.g.) for 9 weeks. The kidney was fixed in 10% formalin for glomerulus fibrosis examination using Masson trichrome staining. Kidney and blood were obtained for assays of the associated biochemical parameters. Chronic Mangiferin treatment prevented renal glomerulus fibrosis evidenced by decreases in Mason-stained positive area of glomeruli, protein expression of type IV collagen, and α-smooth muscle actin in the kidney of diabetic rats, in comparison with decreases in mRNA and protein expression of osteopontin as well as protein expression of cyclooxygenase 2 and NF-кB p65 subunit in the renal cortex of diabetic rats. Moreover, Mangiferin reduced the levels of interleukin 1β in both the serum and the kidney of diabetic rats.
CONCLUSIONS:
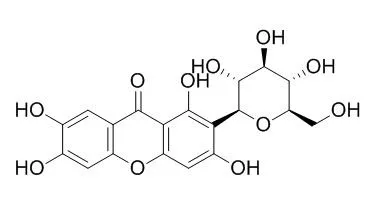
Our findings demonstrate that Mangiferin prevents the renal glomerulus fibrosis of diabetic rats, which is realized through the suppression of osteopontin overproduction and inflammation likely via inactivation of NF-кB. | | Toxicol Appl Pharmacol. 2014 Oct 15;280(2):207-15. | | Mangiferin treatment inhibits hepatic expression of acyl-coenzyme A:diacylglycerol acyltransferase-2 in fructose-fed spontaneously hypertensive rats: a link to amelioration of fatty liver.[Pubmed: 25123789] | Mangiferin, a xanthone glucoside, and its associated traditional herbs have been demonstrated to improve abnormalities of lipid metabolism. However, its underlying mechanisms remain largely unclear.
METHODS AND RESULTS:
This study investigated the anti-steatotic effect of Mangiferin in fructose-fed spontaneously hypertensive rat (SHR)s that have a mutation in sterol regulatory element binding protein (SREBP)-1. The results showed that co-administration of Mangiferin (15 mg/kg, once daily, by oral gavage) over 7 weeks dramatically diminished fructose-induced increases in hepatic triglyceride content and Oil Red O-stained area in SHRs. However, blood pressure, fructose and chow intakes, white adipose tissue weight and metabolic parameters (plasma concentrations of glucose, insulin, triglyceride, total cholesterol and non-esterified fatty acids) were unaffected by Mangiferin treatment. Mechanistically, Mangiferin treatment suppressed acyl-coenzyme A:diacylglycerol acyltransferase (DGAT)-2 expression at the mRNA and protein levels in the liver. In contrast, Mangiferin treatment was without effect on hepatic mRNA and/or protein expression of SREBP-1/1c, carbohydrate response element binding protein, liver pyruvate kinase, fatty acid synthase, acetyl-CoA carboxylase-1, stearoyl-CoA desaturase-1, DGAT-1, monoacyglycerol acyltransferase-2, microsomal triglyceride transfer protein, peroxisome proliferator-activated receptor-alpha, carnitine palmitoyltransferase-1 and acyl-CoA oxidase.
CONCLUSIONS:
Collectively, our results suggest that Mangiferin treatment ameliorates fatty liver in fructose-fed SHRs by inhibiting hepatic DGAT-2 that catalyzes the final step in triglyceride biosynthesis. The anti-steatotic effect of Mangiferin may occur independently of the hepatic signals associated with de novo fatty acid synthesis and oxidation. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)