| Description: |
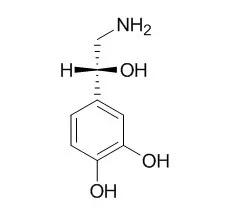
Norepinephrine is a peripheral vasoconstrictor by acting on alpha-adrenergic receptors, it can up-regulate the expression of vascular endothelial growth factor, matrix metalloproteinase (MMP)-2, and MMP-9 in nasopharyngeal carcinoma tumor cells. Norepinephrine can stimulates apoptosis in adult rat ventricular myocytes by activation of the β-adrenergic pathway. Noradrenergic system may play a significant role in modulating the development of ischemic neuronal damage. |
| Targets: |
VEGFR | Sodium Channel | MMP(e.g.TIMP) |
| In vitro: |
| Am J Physiol Renal Physiol. 2015 Mar 1;308(5):F450-8. | | Norepinephrine stimulates the epithelial Na+ channel in cortical collecting duct cells via α2-adrenoceptors.[Pubmed: 25520009] | There is good evidence for a causal link between excessive sympathetic drive to the kidney and hypertension. We hypothesized that sympathetic regulation of tubular Na(+) absorption may occur in the aldosterone-sensitive distal nephron, where the fine tuning of renal Na(+) excretion takes place.
METHODS AND RESULTS:
Here, the appropriate regulation of transepithelial Na(+) transport, mediated by the amiloride-sensitive epithelial Na(+) channel (ENaC), is critical for blood pressure control. To explore a possible effect of the sympathetic transmitter Norepinephrine on ENaC-mediated Na(+) transport, we performed short-circuit current (Isc) measurements on confluent mCCDcl1 murine cortical collecting duct cells. Norepinephrine caused a complex Isc response with a sustained increase of amiloride-sensitive Isc by ∼44%. This effect was concentration dependent and mediated via basolateral α2-adrenoceptors. In cells pretreated with aldosterone, the stimulatory effect of Norepinephrine was reduced. Finally, we demonstrated that noradrenergic nerve fibers are present in close proximity to ENaC-expressing cells in murine kidney slices.
CONCLUSIONS:
We conclude that the sustained stimulatory effect of locally elevated Norepinephrine on ENaC-mediated Na(+) absorption may contribute to the hypertensive effect of increased renal sympathetic activity. | | Circulation. 1998 Sep 29;98(13):1329-34. | | Norepinephrine stimulates apoptosis in adult rat ventricular myocytes by activation of the beta-adrenergic pathway.[Pubmed: 9751683] |
METHODS AND RESULTS:
Myocytes were exposed to NE alone (10 micromol/L), NE+propranolol (2 micromol/L), NE+prazosin (0.1 micromol/L), or isoproterenol (ISO, 10 micromol/L) for 24 hours. NE and ISO decreased the number of viable myocytes by approximately 35%. This effect was completely blocked by the beta-adrenergic antagonist propranolol but was not affected by the alpha1-adrenergic antagonist prazosin. NE increased DNA laddering on agarose gel electrophoresis and increased the percentage of cells that were stained by terminal deoxynucleotidyl transferase-mediated nick end-labeling from 5.8+/-1. 0% to 21.0+/-2.3% (P<0.01; n=4). NE likewise increased the percentage of apoptotic cells with hypodiploid DNA content as assessed by flow cytometry from 7.8+/-0.7% to 16.7+/-2.2% (P<0.01; n=6), and this effect was abolished by propranolol but not prazosin. ISO and forskolin (10 micromol/L) mimicked the effect of NE, increasing the percentage of apoptotic cells to 14.7+/-1.9% and 14. 4+/-2.2%, respectively. NE-stimulated apoptosis was abolished by the protein kinase A inhibitor H-89 (20 micromol/L) or the voltage-dependent calcium channel blockers diltiazem and nifedipine.
CONCLUSIONS:
NE, acting via the ss-adrenergic pathway, stimulates apoptosis in adult rat cardiac myocytes in vitro. This effect is mediated by protein kinase A and requires calcium entry via voltage-dependent calcium channels. NE-stimulated apoptosis of cardiac myocytes may contribute to the progression of myocardial failure. |
|
| In vivo: |
| Anesthesiology. 2015 Apr;122(4):736-45. | | Randomized double-blinded comparison of norepinephrine and phenylephrine for maintenance of blood pressure during spinal anesthesia for cesarean delivery.[Pubmed: 25635593 ] | During spinal anesthesia for cesarean delivery, phenylephrine can cause reflexive decreases in maternal heart rate and cardiac output. Norepinephrine has weak β-adrenergic receptor agonist activity in addition to potent α-adrenergic receptor activity and therefore may be suitable for maintaining blood pressure with less negative effects on heart rate and cardiac output compared with phenylephrine.
METHODS AND RESULTS:
In a randomized, double-blinded study, 104 healthy patients having cesarean delivery under spinal anesthesia were randomized to have systolic blood pressure maintained with a computer-controlled infusion of Norepinephrine 5 μg/ml or phenylephrine 100 μg/ml. The primary outcome compared was cardiac output. Blood pressure heart rate and neonatal outcome were also compared. Normalized cardiac output 5 min after induction was greater in the Norepinephrine group versus the phenylephrine group (median 102.7% [interquartile range, 94.3 to 116.7%] versus 93.8% [85.0 to 103.1%], P = 0.004, median difference 9.8%, 95% CI of difference between medians 2.8 to 16.1%). From induction until uterine incision, for Norepinephrine versus phenylephrine, systolic blood pressure and stroke volume were similar, heart rate and cardiac output were greater, systemic vascular resistance was lower, and the incidence of bradycardia was smaller. Neonatal outcome was similar between groups.
CONCLUSIONS:
When given by computer-controlled infusion during spinal anesthesia for cesarean delivery, Norepinephrine was effective for maintaining blood pressure and was associated with greater heart rate and cardiac output compared with phenylephrine. Further work would be of interest to confirm the safety and efficacy of Norepinephrine as a vasopressor in obstetric patients. |
|

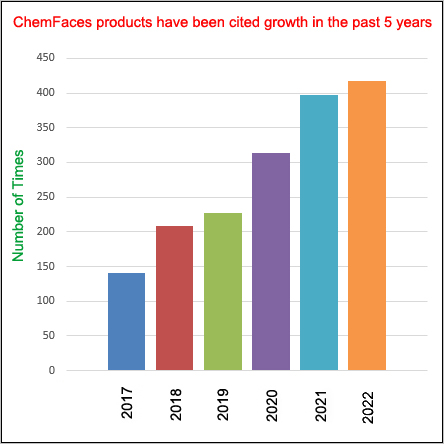

 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)