| In vitro: |
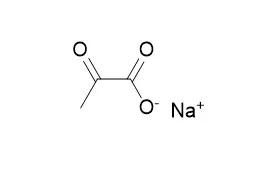
| Journal of Chemical Neuroanatomy, 2003, 26(2):109-118. | | Sodium pyruvate protects against H(2)O(2) mediated apoptosis in human neuroblastoma cell line-SK-N-MC.[Pubmed: 14599660] | Free radicals are involved in neuronal damage.
METHODS AND RESULTS:
The present study was aimed to investigate the protective effect of Sodium pyruvate-a free radical scavenger against hydrogen peroxide (H(2)O(2)) induced apoptosis in human neuroblastoma cell line-SK-N-MC. On exposure to H(2)O(2) (0.025 mM) cells exhibited apoptosis within 24 h, demonstrating a high caspase 3 activity by 3 h followed by cleavage of PARP that was maximum at 24 h. A break down in the mitochondrial membrane potential was observed 3 h onwards. Sodium pyruvate protected cells significantly (P<0.05) against apoptosis in a dose dependent manner as assessed for cell viability by dye exclusion method and apoptosis by TUNEL. Sodium pyruvate significantly inhibited caspase 3 activity, cleavage of PARP and breakdown of mitochondrial membrane potential.
CONCLUSIONS:
These data suggest that Sodium pyruvate protects neuronal damage caused by H(2)O(2). | | International Journal of Molecular Medicine, 2016,37(2): 517-525. | | Ethanol, ethyl and sodium pyruvate decrease the inflammatory responses of human lung epithelial cells via Akt and NF-κB in vitro but have a low impact on hepatocellular cells.[Reference: WebLink] | Increases in pro-inflammatory cytokine levels and tissue-infiltrating leukocytes have been closely linked to increased systemic and local inflammation, which result in organ injury. Previously, we demonstrated the beneficial and hepatoprotective anti-inflammatory effects of acute ethanol (EtOH) ingestion in an in vivo model of acute inflammation. Due to its undesirable side-effects, however, EtOH does not represent a therapeutic option for treatment of acute inflammation.
METHODS AND RESULTS:
Therefore, in this study, we compared the effects of acute EtOH exposure with ethyl pyruvate (EtP) as an alternative anti-inflammatory drug in an in vitro model of hepatic and pulmonary inflammation. Human hepatocellular carcinoma cells Huh7 and alveolar epithelial cells A549 were stimulated with either interleukin (IL) IL-1β (1 ng/ml, 24 h) or tumor necrosis factor (TNF) (10 ng/ml, 4 h), and then treated with EtP (2.5-10 mM), Sodium pyruvate (NaP, 10 mM) or EtOH (85-170 mM) for 1 h. IL-6 or IL-8 release from Huh7 or A549 cells, respectively, was measured by an enzymelinked immunosorbent assay. Neutrophil adhesion to cell monolayers and CD54 expression were also analyzed. Bcl-2 and Bax gene expression was determined by RT-qPCR, and western blot analysis was performed to determine the mechanisms involved. Treating A549 cells with either EtOH or EtP significantly reduced the IL-1β- or TNFinduced IL-8 release, whereas treating Huh7 cells did not significantly alter IL-6 release. Similarly, neutrophil adhesion to stimulated A549 cells was significantly reduced by EtOH or EtP, whereas for Huh7 cells the tendency for reduced neutrophil adhesion rates by EtOH or EtP was not significant. CD54 expression was noticeably reduced in A549 cells, but this was not the case in Huh7 cells after treatment. The Bax/Bcl-2 ratio was dosedependently decreased by EtOH and by high-dose EtP in A549 cells, indicating a reduction in apoptosis, whereas this effect was not observed in Huh7 cells. The underlying mechanisms involve reduced phosphorylation of Akt and nuclear factor-κB (NF-κB) p65. We noted that as with EtP, EtOH reduced the inflammatory response in lung epithelial cells under acute inflammatory conditions.
CONCLUSIONS:
However, due to the low impact which EtP and EtOH had on the hepatocellular cells, our data suggest that both substances exerted different effects depending on the cellular entity. The possible underlying mechanisms involved the downregulation of Akt and the transcription factor NF-κB, but further research on this subject is required. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)