| Animal Research: |
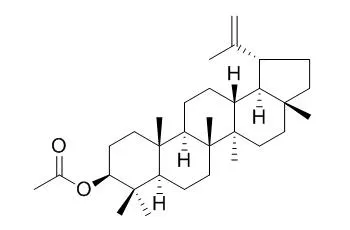
| J. Inflamm. (Lond). 2010; 7: 60. | | Anti-inflammatory effects and possible mechanism of action of lupeol acetate isolated from Himatanthus drasticus (Mart.) Plumel.[Pubmed: 21167055] | The species Himatanthus drasticus is popularly known in Northeast Brazil as "janaguba" and belongs to the family Apocynaceae. The latex collected from its stem bark is used for several purposes including anti-inflammatory properties and presents among its bioactive constituents the pentacyclic triterpene lupeol. The objective of the present work was to study in vivo and in vitro the Lupeol acetate (LA) isolated from the plant latex, in several models of inflammation.
METHODS AND RESULTS:
Male Swiss mice (25-30 g, 6-24 animals per group) were administered with LA, 30 min before the test initiation. In the evaluation of analgesic activity the formalin test was used. The anti-inflammatory activity was evaluated by the following tests: paw edema induced by carrageenan and dextran, and the carrageenan-induced neutrophil migration into peritoneal cavities. Furthermore, the effect of LA on the myeloperoxidase release (MPO, an inflammation biomarker) from human neutrophils was also determined, as well as its antioxidant potential by the DPPH assay.
In the formalin test, LA (10, 25 and 50 mg/kg, i.p.) inhibited both the 1st (neurogenic, 0-5 min) and mainly the 2nd (inflammatory, 20-25 min) phase. Naloxone completely reversed the LA effect, indicating the participation of the opioid system. LA also significantly inhibited carrageenan- and dextran-induced paw edemas, as well as the neutrophil migration to the peritoneal cavity evaluated by the carrageenan-induced pleurisia. In this model, the effect of a very low dose of LA (0.1 mg/kg) was potentiated by the same dose of pentoxifylline (PTX), a known TNF-alpha inhibitor. LA (25 and 50 μg/ml) was also very effective in inhibiting MPO released from stimulated human neutrophils, and significantly decreased the number of cells expressing iNOS activity in the paw of mice submitted to carrageenan-induced edema, suggesting a drug involvement with the NO system.
CONCLUSIONS:
The anti-inflammatory effect of LA probably involves the opioid system, as indicated by the complete blockade of the opioid antagonist naloxone. Furthermore, the LA effect was potentiated by PTX (a TNF-alpha inhibitor). LA also decreased the number of iNOS cells, suggesting the participation of pro-inflammatory cytokines and the NO system in the drug action. | | Biomed Pharmacother. 2016 Apr;79:231-40. | | Lupeol acetate ameliorates collagen-induced arthritis and osteoclastogenesis of mice through improvement of microenvironment.[Pubmed: 27044833 ] | Lupeol has been shown with anti-inflammation and antitumor capability, however, the poor bioavailability limiting its applications in living subjects. Lupeol acetate (LA), a derivative of lupeol, shows similar biological activities as lupeol but with better bioavailability.
METHODS AND RESULTS:
Here RAW 264.7 cells and bone marrow-derived macrophages (BMDMs) stimulated by lipopolysaccharide (LPS) were treated with 0-80μM of LA, and assayed for TNF-α, IL-1β, COX-2, MCP-1 using Western blotting. Moreover, osteoclatogenesis was examined with reverse transcription PCR (RT-PCR) and tartrate-resistant acid phosphatase (TRAP) staining. For in vivo study, collagen-induced arthritis (CIA)-bearing DBA/1J mice were randomly separated into three groups: vehicle, LA-treated (50mg/kg) and curcumin-treated (100mg/kg). Therapeutic efficacies were assayed by the clinical score, expression levels of serum cytokines including TNF-α and IL-1β, (18)F-fluorodeoxyglucose ((18)F-FDG) microPET/CT and histopathology.
CONCLUSIONS:
The results showed that LA could inhibit the activation, migration, and formation of osteoclastogenesis of macrophages in a dose-dependent manner. In RA-bearing mice, the expressions of inflammation-related cytokines were suppressed, and clinical symptoms and bone erosion were ameliorated by LA. The accumulation of (18)F-FDG in the joints of RA-bearing mice was also significantly decreased by LA. The results indicate that LA significantly improves the symptoms of RA by down-regulating expressions of inflammatory cytokines and osteoclastogenesis. |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)