| In vitro: |
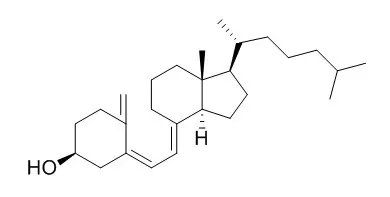
| J Pharm Biomed Anal. 2014 Mar;91:73-80. | | Development of a validated UPLC method for simultaneous estimation of both free and entrapped (in solid lipid nanoparticles) all-trans retinoic acid and cholecalciferol (vitamin D3) and its pharmacokinetic applicability in rats.[Pubmed: 24440824] | A sensitive ultra-performance liquid chromatography (UPLC) method was developed for simultaneous estimation of all-trans retinoic acid (ATRA) and cholecalciferol (Vitamin D3) in rat plasma.
METHODS AND RESULTS:
The method was validated over the linear range of 1.0-5000ng/ml (r(2)=0.999) for both vitamins with a limit of detection of 0.5ng/ml. Chromatographic separation was achieved using liquid-liquid extraction (LLE) on an Acquity BEH RP 18 column (2.1mm×50mm, I.D. 1.7μm), with mobile phase comprising of acetonitrile:methanol:water (90:8:2, v/v/v), at a flow rate of 0.20ml/min and a total run time of 5min. Intra and inter-day variability (RSD) was ≤3.1%, and the accuracy varied between 95.4-99.9% and 95.3-101.1% respectively, for ATRA and 98.5-100.8% and 99.3-101.7%, respectively for Vitamin D3. High recovery of ≥96.0% for ATRA and ≥87.80% for Vitamin D3 was achieved. ATRA and Vitamin D3 were stable in plasma under different storage and processing conditions. The method was applied to estimate the total drug content and entrapment efficiency of ATRA and Vitamin D3 loaded solid lipid nanoparticles (SLNs). Concentration of these two agents was determined in rat plasma after simultaneous subcutaneous administration in free form or when loaded into SLNs thus establishing pharmacokinetic application of the developed procedure.
CONCLUSIONS:
Results indicated an improvement in AUC0-∞ by 5.4 times and 29.4 times for ATRA and Vitamin D3, respectively, upon their incorporation into SLNs. Simultaneous administration of these two vitamins and their improved and prolonged bioavailability has scope for their use in treatment and control of tuberculosis. |
|
| In vivo: |
| Eur J Endocrinol. 2015 Mar;172(3):235-41. | | Vitamin D3 increases in abdominal subcutaneous fat tissue after supplementation with vitamin D3.[Pubmed: 25661743] | The objective was to assess the amount of Vitamin D3 stored in adipose tissue after long-term supplementation with high dose Vitamin D3.
A cross-sectional study on 29 subjects with impaired glucose tolerance who had participated in a randomized controlled trial with Vitamin D3 20 000 IU (500 μg) per week vs placebo for 3-5 years.
METHODS AND RESULTS:
Abdominal subcutaneous fat tissue was obtained by needle biopsy for the measurements of Vitamin D3 and 25-hydroxyVitamin D3 (25(OH)D3). Body fat was measured with dual-energy X-ray absorptiometry, and serum 25(OH)D3 level was quantified.
In the subjects given Vitamin D3, the median concentrations of serum 25(OH)D3, fat Vitamin D3, and fat 25(OH)D3 were 99 nmol/l, 209 ng/g, and 3.8 ng/g, respectively; and correspondingly in the placebo group 62 nmol/l, 32 ng/g, and 2.5 ng/g. If assuming an equal amount of Vitamin D3 stored in all adipose tissue in the body, the median body store was 6.6 mg Vitamin D3 and 0.12 mg 25(OH)D3 in those given Vitamin D3.
CONCLUSIONS:
Subcutaneous adipose tissue may store large amounts of Vitamin D3. The clinical importance of this storage needs to be determined. | | J Steroid Biochem Mol Biol. 2015 Apr;148:275-82. | | Dissecting high from low responders in a vitamin D3 intervention study.[Pubmed: 25448738] | Vitamin D3 is a pleiotropic signaling molecule that has via activation of the transcription factor vitamin D receptor (VDR) a direct effect on the expression of more than 100 genes. The aim of this study was to find transcriptomic and clinical biomarkers that are most suited to identify Vitamin D3 responders within 71 pre-diabetic subjects during a 5-month intervention study (VitDmet).
METHODS AND RESULTS:
In hematopoietic cells, the genes ASAP2, CAMP, CD14, CD97, DUSP10, G0S2, IL8, LRRC8A, NINJ1, NRIP1, SLC37A2 and THBD are known as primary vitamin D targets. We demonstrate that each of these 12 genes carries a conserved VDR binding site within its genomic region and is expressed in human peripheral blood mononuclear cells (PBMCs). The changes in the expression of these genes in human PBMCs at the start and the end of the vitamin D-intervention were systematically correlated with the alteration in the circulating form of Vitamin D3, 25-hydroxyVitamin D3 (25(OH)D3). Only 39-44 (55-62%) of the study subjects showed a highly significant response to Vitamin D3, i.e., we considered them as "responders". In comparison, we found for 37-53 (52-75%) of the participants that only 12 biochemical and clinical parameters, such as concentrations of parathyroid hormone (PTH) and insulin, or computed values, such as homeostatic model assessment and insulin sensitivity index, show a correlation with serum 25(OH)D3 levels that is as high as that of the selected VDR target genes. All 24 parameters together described the pleiotropic vitamin D response of the VitDmet study subjects. Interestingly, they demonstrated a number of additional correlations that define a network, in which PTH plays the central role.
CONCLUSIONS:
In conclusion, Vitamin D3-induced changes in human PBMCs can be described by transcriptomic and serum biomarkers and allow a segregation into high and low responders. This article is part of a Special Issue entitled '17th Vitamin D Workshop' . |
|





 Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019)
Cell. 2018 Jan 11;172(1-2):249-261.e12. doi: 10.1016/j.cell.2017.12.019.IF=36.216(2019) Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019)
Cell Metab. 2020 Mar 3;31(3):534-548.e5. doi: 10.1016/j.cmet.2020.01.002.IF=22.415(2019) Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)
Mol Cell. 2017 Nov 16;68(4):673-685.e6. doi: 10.1016/j.molcel.2017.10.022.IF=14.548(2019)